A Real Heartache
The Case
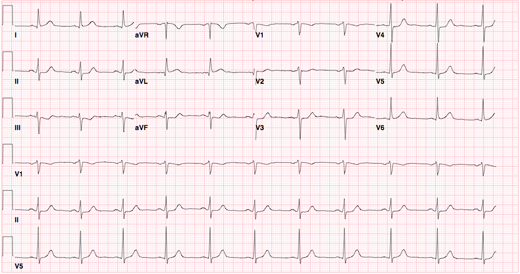
A 60-year-old man presented to the emergency department (ED) with 2 hours of burning chest pain. The pain began at rest, and it radiated to his back and left axilla. He had no other complaints and reported being in good health otherwise. His past medical history was notable for a history of depression, a 40-pack/year history of cigarette smoking, and a father who had a heart attack at age 49. On physical examination, his initial blood pressure was elevated at 192/100 mm Hg, but his heart rate and the rest of his cardiopulmonary examination were normal. Bilateral upper-extremity blood pressures were equal. An electrocardiogram (ECG) was obtained (Figure 1) and interpreted as unremarkable. A chest radiograph and routine blood work, including a troponin assay, were also normal. The patient received aspirin and sublingual nitroglycerin without symptom improvement. Subsequently, a "GI cocktail" (an oral antacid/anesthetic combination) was given, and the patient reported symptom relief; his blood pressure also normalized. Convinced that a cardiac etiology had been ruled out because of the atypical pain, the unremarkable ECG, the normal troponin, and the response to the GI cocktail, the ED physician discharged the patient to home with a presumptive diagnosis of gastroesophageal reflux disease (GERD). The patient was advised to follow up with his primary care physician.
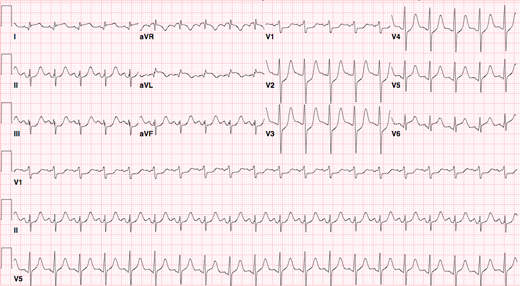
Two days later, the patient made an unscheduled return visit to the ED, now in severe distress. He complained of abdominal pain and was dyspneic, hypotensive, and with mottled skin. Fluid and pressor support was initiated, and the patient was intubated. ED physicians obtained an ECG (Figure 2), which showed ST-segment elevation, prompting urgent cardiology consultation with concern for an acute myocardial infarction and/or aortic dissection. A bedside echocardiogram revealed a large pericardial effusion, and the patient was taken urgently to the cardiac catheterization lab. Cardiac catheterization showed branch occlusion of the left circumflex coronary artery. The patient stabilized and further evaluation did not reveal a myocardial rupture. Two days later, the patient had a cardiac arrest and could not be resuscitated. An autopsy revealed 3-vessel atherosclerotic coronary artery disease and a 4-day-old transmural myocardial infarct with extension and associated rupture of the left ventricular free wall. The consensus of the ED quality committee's case review was that the patient had a diagnosis of myocardial infarction, which was missed at his initial presentation.
The Commentary
Chest pain is one of the most common chief complaints in emergency departments (EDs), constituting 5% of all visits.(1) There are both immediately life-threatening etiologies (e.g., acute coronary syndrome, aortic dissection, pulmonary embolus) and benign ones (e.g., costochondritis, gastroesophageal reflux disease, panic disorder), but symptoms overlap considerably, which makes differentiating between them anything but straightforward. Acute coronary syndromes (ACS) include acute myocardial infarction (AMI) and unstable angina and typically constitute 15% of all patients with undifferentiated chest pain in the ED. Given this prevalence, the risk to patients, and the medicolegal risk to clinicians of missing an AMI, considerable effort is made in identifying or excluding these syndromes.
The tools immediately available to assist clinicians in identifying ACS include the history, physical examination, ECG, and cardiac biomarkers. If the initial ECG and/or cardiac biomarkers are indicative of infarction, then treatment for ST elevation or non-ST elevation myocardial infarction is initiated. This treatment may include percutaneous coronary intervention, fibrinolytic therapy, and antiplatelet agents. In the absence of overt infarction, further ED testing is routinely employed.
The case presented provides a sobering reminder of the limitations of our available tools and our own cognitive processes in interpreting them. It's also a helpful reminder about how retrospective case reviews can capture not only individual provider concerns but also system-level issues that could prevent similar events from recurring.
Case Review: Identifying Errors and Contributing Factors
In this case, the clinicians believed that the quality of the patient's pain was "atypical" for cardiac ischemia, and thus they considered the likelihood of this diagnosis less probable. Multiple studies have considered the quality of the pain in relation to the ultimate diagnosis of myocardial infarction or ischemia. Burning pain has not been associated with a reduced likelihood of ischemia; whereas, sharp, pleuritic, or positional pain is associated with a significantly lower risk (likelihood ratios [LR] of 0.2 to 0.3).(2) Interestingly, a United Kingdom-based study noted that indigestion or burning type pain was in fact predictive of ACS.(3)
Another contributing factor to the missed diagnosis in this case was that the initial ECG was interpreted as unremarkable. A normal ECG does reduce the probability of a myocardial infarct (LR of 0.1 to 0.3).(2) Careful inspection of Figure 1 does reveal non-specific ST/T changes, but it's unclear whether the providers had a baseline ECG available for comparison. In a study of patients that presented to 10 EDs with chest pain or an equivalent, a normal or non-diagnostic ECG significantly increased the odds of inappropriate discharge (odds ratio [OR] 7.7, 95% confidence interval [CI] 2.9 to 20.2) for patients ultimately proven to have a myocardial infarct.(4) In this same study, the authors suggested that improved ECG reading skills might have identified the 2% of patients that were prematurely discharged with an AMI.
To reassure them regarding the absence of cardiac ischemia, the clinicians in this case seemed to rely on the results of a diagnostic trial: no response to nitroglycerin vs. relief after an oral antacid/anesthetic solution. This approach is not validated; in fact, response to either medication has been found to be misleading. The reduction of chest discomfort by sublingual nitroglycerin as a predictor of ischemic chest pain is confounded by both the placebo effect and its property of causing smooth muscle relaxation (which may improve the pain of esophageal spasm).(5) Furthermore, several small studies document either partial or complete relief of chest discomfort with oral antacid solutions in the presence of occlusive coronary artery disease.(6)
In the case presented above, clinicians did not follow an algorithmic and evidence-based approach to the evaluation of chest pain. Given that the clinicians considered the possibility that the pain was ischemic in nature and the patient had several established risk factors for coronary artery disease (e.g., untreated hypertension, cigarette smoking, and premature family history), serial sampling of cardiac biomarkers and ECG tracings was indicated.(7) The Thrombolysis in Myocardial Infarction (TIMI) risk score is a validated tool in ED chest pain patients and useful to risk stratify and guide further therapy.(8,9) This patient had a TIMI score of 1 (Table), which translates to an 8.2% (95% CI 5.27 to 11.04) incidence of cardiovascular morbidity or mortality at 30 days—clearly too high to merit reassurance and discharge.
What should have been done in this case? The patient should have remained in the ED (or observation unit, if available) for a minimum of 6 hours longer and received an additional ECG and cardiac biomarker test.(7) The extra time takes into account the sensitivity of the cardiac biomarker assay in early presentations such as this. If either had turned positive, he should have been admitted for management of ACS. If they remained negative, he should have undergone further testing. Reasonable options would have been either immediate stress testing, expedited outpatient stress testing (in the next 1 to 2 days), or expedited coronary computed tomographic (CT) angiography. The latter technology is a noninvasive test with excellent test characteristics to exclude coronary artery disease (negative predictive value of nearly 100%, LR of 0.06) in ED patients with chest pain.(10,11) In our ED, we would have favored immediate exercise stress testing, but all of these strategies are acceptable and evidence-based. Final disposition and management is determined by the results of these tests.
Borrowing from cognitive psychology, it appears that the management of this patient is a demonstration of confirmation bias, where one has a tendency to focus on evidence that supports a working diagnosis rather than consider evidence that tends to refute it.(12) Once the ED physician settled on a working diagnosis of a non-cardiac etiology, the addition of a positive response to an antacid served to confirm a gastrointestinal diagnosis. Given the benign nature of this diagnosis, the clinician did not pursue any further workup or evaluation and discharged the patient. In retrospect, this was the wrong decision. Whether or not the death of this patient could have been prevented is conjecture, but further consideration of alternative life-threatening diagnoses would have been prudent.
Take-Home Points
- In patients with chest pain, careful interpretation of the ECG and comparison with previous tracings is essential.
- Reliance on the response of chest pain to diagnostic trials, such as to nitroglycerin or oral antacids, is not evidence-based and may be misleading.
- In patients without overt ischemic changes or evidence of infarction on ECG or initial biomarker testing, serial tracings and biomarker testing followed by either immediate or expedited stress testing should be the norm.
- Systematic use of a risk stratification score, such as the TIMI score, can help ensure appropriate decision-making in the ED and guard against being unduly influenced by our cognitive biases.
- Coronary CT angiography is an emerging strategy to definitively identify or exclude coronary artery disease and should be considered.
Steven K. Polevoi, MD Clinical Professor of Emergency Medicine Medical Director, Emergency Department Department of Emergency Medicine University of California, San Francisco
References
1. Nawar EW, Niska RW, Xu J. National Hospital Ambulatory Medical Case Survey: 2005 emergency department summary. Adv Data. 2007;(386):1-32. [go to PubMed]
2. Panju AA, Hemmelgarn BR, Guyatt GH, Simel DL. Is this patient having a myocardial infarction? JAMA. 1998;280:1256-1263. [go to PubMed]
3. Goodacre SW, Angelini K, Arnold J, Revill S, Morris F. Clinical predictors of acute coronary syndromes in patients with undifferentiated chest pain. QJM. 2003;96:893-898. [go to PubMed]
4. Pope JH, Aufderheide TP, Ruthazer R, et al. Missed diagnosis of acute cardiac ischemia in the emergency department. N Engl J Med. 2000;342:1163-1170. [go to PubMed]
5. Diercks DB, Boghos E, Guzman H, Amsterdam EA, Kirk JD. Changes in the numeric descriptive scale for pain after sublingual nitroglycerin do not predict cardiac etiology of chest pain. Ann Emerg Med. 2005;45:581-585. [go to PubMed]
6. Wrenn K, Slovis CM, Gongaware J. Using the "GI cocktail": a descriptive study. Ann Emerg Med. 1995;26:687-690. [go to PubMed]
7. Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non–ST-elevation myocardial infarction: executive summary. Circulation. 2007;116:803-877. [Available at]
8. Chase M, Robey JL, Zogby KE, Sease KL, Shofer FS, Hollander JE. Prospective validation of the Thrombosis in Myocardial Infarction Risk Score in the emergency department chest pain population. Ann Emerg Med. 2006;48:252-259. [go to PubMed]
9. Hess EP, Agarwal D, Chandra S, et al. Diagnostic accuracy of the TIMI risk score in patients with chest pain in the emergency department: a meta-analysis. CMAJ. 2010;182:1039-1044. [go to PubMed]
10. Hoffmann U, Truong QA, Schoenfeld DA, et al; ROMICAT-II Investigators. Coronary CT angiography versus standard evaluation in acute chest pain. N Engl J Med. 2012;67:299-308. [go to PubMed]
11. Budoff MJ, Dowe D, Jollis JG, et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol. 2008;52:1724-1732. [go to PubMed]
12. Croskerry P. The importance of cognitive errors in diagnosis and strategies to minimize them. Acad Med. 2003;78:775-780. [go to PubMed]
Table
Table. Predictor variables included in the TIMI risk score*.(9)| • Age 65 years or older |
| • Three or more risk factors for atherosclerosis |
| • Known coronary artery disease (> 50% stenosis) |
| • Two or more anginal episodes in the preceding 24 hours |
| • Aspirin use in the 7 days prior to presentation |
| • ST-segment deviation of 0.05 mV or more |
| • Elevated cardiac markers |
*To calculate the TIMI risk score, sum the number of positive predictor variables (0–7).
Figures
Figure 1. Initial ECG. ECG interpretation: NSR with non-specific ST/T wave changes.
Figure 2. Repeat ECG at return ED visit. ECG interpretation: sinus tachycardia, with posterolateral injury pattern.