Strongyloides: A Hidden Traveler and Potentially Lethal Missed Diagnosis.
Carlile N, Smith CL, Maguire JH, et al. Strongyloides: A Hidden Traveler and Potentially Lethal Missed Diagnosis.. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2022.
Carlile N, Smith CL, Maguire JH, et al. Strongyloides: A Hidden Traveler and Potentially Lethal Missed Diagnosis.. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2022.
Patrick Romano, MD, MPH; Debra Bakerjian, PhD, APRN, RN; Narath Carlile, MD, MPH; James H. Maguire, MD; Gordon David Schiff, MD; Ulfat Shaikh, MD; Clyde Lanford Smith, MD, MPH, DTM&H for this Spotlight Case and Commentary have disclosed no relevant financial relationships with ineligible companies related to this CME activity.
Learning Objectives
At the conclusion of this educational activity, participants should be able to:
- Recognize common and serious pitfalls in diagnosis of Strongyloides and potential consequences of failure to diagnose this infection.
- Summarize approaches to diagnosis and treatment of Strongyloides infection.
- Identify patients who should be tested for Strongyloides infection.
The Case
A man in his 70s with a history of multiple myeloma (a cancer of the bone marrow), high blood pressure, osteoporosis, and pulmonary embolus, was admitted to a hospital with gastrointestinal symptoms and diagnosed with cholecystitis (a severe infection of his gallbladder), which was treated surgically with the finding of gangrenous gallbladder.
He was originally from Haiti and moved to the United States in the 1980s. Prior to his current illness he frequently traveled to see his family in Haiti, the Dominican Republic, and several countries in Central America. He had been seen numerous times for diarrhea in the previous five years, but the diarrhea had always been attributed to viral or unknown causes, without any microbiologic or serologic testing. His eosinophil counts were intermittently elevated during these 5 years, a finding that was either not noted or not commented upon by the physicians who treated him. One physician attributed his eosinophilia to lenalinomide, a medication that he had previously received for treatment of multiple myeloma. His treatment of multiple myeloma also included long periods on dexamethasone, but he was no longer taking either lenalinomide or dexamethasone at admission.
Two months after his admission for cholecystitis, he was again seen with severe vomiting, was found to be hypotensive, and was readmitted to the hospital. An upper gastrointestinal endoscopy was done. Biopsies unexpectedly showed that his duodenum was heavily infiltrated with a parasitic helminth (worm) called Strongyloides stercoralis. He was treated with the anti-parasitic drug ivermectin and eventually improved enough to be discharged from the hospital.
The Commentary
By Narath Carlile, MD, MPH, Clyde Lanford Smith, MD, MPH, DTM&H, James H. Maguire, MD, and Gordon D. Schiff, MD
Pathophysiology
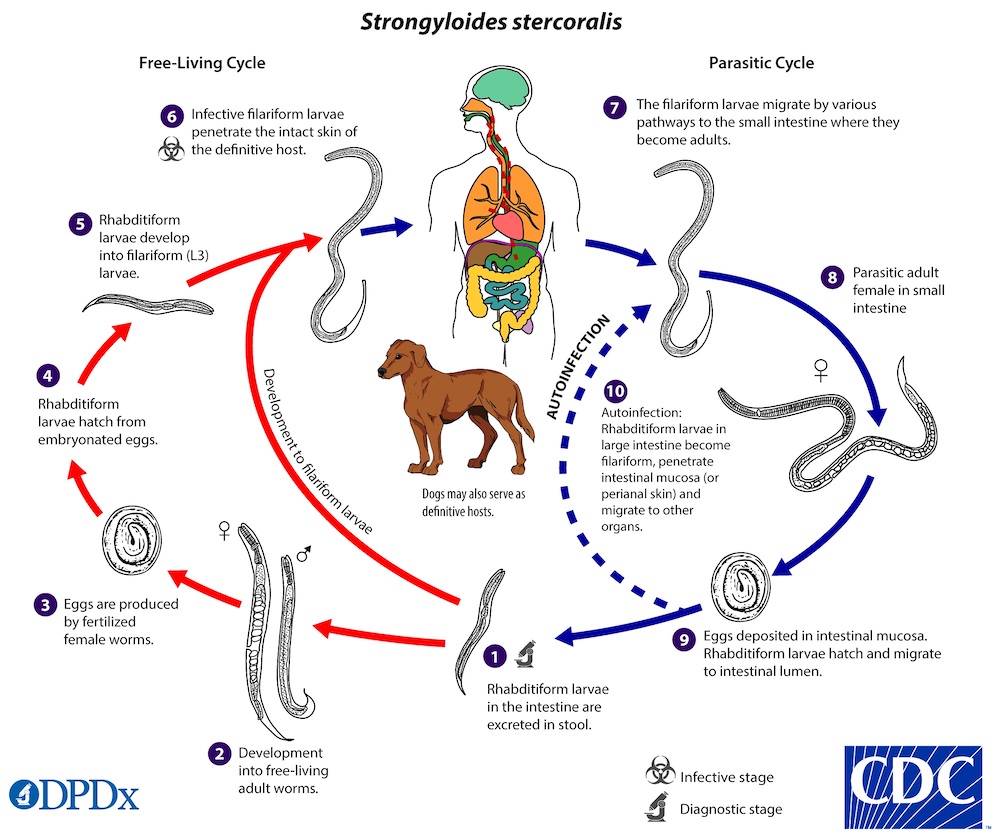
Strongyloides stercoralis is a helminth that is endemic to tropical and subtropical regions of the world, across Central and South America, Africa, and Asia. In the classic but usually silent life cycle (Figure 1), the larval worm typically enters the body from people walking with bare feet on contaminated soil, or by contact with human waste or sewage. It burrows through the skin, begins maturing to adulthood and travels through the bloodstream to the new host’s lungs. Once in the lungs, it travels up the airway, is swallowed, and penetrates the small bowel mucosa, where it lays eggs that hatch almost immediately, releasing non-infectious larvae. Noninfectious larvae undergo a molt and become infectious either within the gastrointestinal tract or after leaving the body in the feces. Infectious larvae shed in the environment can penetrate human skin; they can also reinfect the same person through the bowel mucosa or the perianal skin and undergo migration through the bloodstream and lungs and back to the gastrointestinal tract. Reinfection can continue throughout the lifetime of the host patient, a process known as autoinfection. Usually, the host’s immune system prevents the number of worms from increasing but cannot clear the infection completely. This results in an ongoing low level of infection, affecting up to 30% of the population in endemic areas, in which the worms continue to release larvae that reinfect the same host or become a source of infection to others.
Figure 1. Life cycle of Strongyloides stercoralis
Image from the CDC DPDx – Laboratory Identification of Parasites of Public Health Concern
If a person’s immune system is weakened, typically by steroids or other immune suppressing medications, viruses such as human T-cell lymphotropic virus type 1 (HTLV-1), or severe malnutrition, Strongyloides replication can increase, leading to a build-up of large numbers of worms, the so-called hyperinfection syndrome. Hyperinfection with Strongyloides is often fatal. While this patient’s intermittent episodes of diarrhea may have been due to strongyloidiasis, he was fortunate not to develop disseminated strongyloidiasis despite receiving several courses of treatment with steroids. It is rare for Strongyloides itself to cause gangrenous cholecystitis and there was reportedly no suggestion of this infection on pathologic examination of the gallbladder specimen. Translocation of Strongyloides larva through the bowel wall (usually lower in the intestine), especially in the setting of delayed intestinal transit, could contribute to bacteremia but is less likely to have been a factor in the present case.
Diagnosis and Treatment
A key issue for this patient was to recognize his risk for Strongyloides infection based on his history of residence and travel. In tropical and subtropical areas, people who live in rural areas with poor sanitation have a greater risk of acquiring strongyloidiasis from fecally contaminated soil than people who live in developed urban areas and are less likely to walk barefoot. Suspecting and testing for Strongyloides is warranted for all patients with these risk factors who are about to start steroids or other immunosuppressive treatment.
Testing in the United States can be done by examination of stool specimens for larvae. However, the sensitivity of a single stool test for detecting larvae is only 30%, and even with multiple specimens reaches only 70-80%. Therefore, screening using an antibody test from a sample of blood is preferred because of its greater sensitivity and specificity, and a positive serological test indicates a high probability of infection.1,2
All persons with positive stool or serological tests should receive treatment with ivermectin, which is highly effective. Other widely used antiparasitic agents, such as albendazole, are less effective. A single dose or two of ivermectin is usually effective for persons with chronic strongyloidiasis, but successful treatment of disseminated infection requires prolonged courses of daily treatment.3,4 One important caveat applies to patients from parts of Central and West Africa, where infection with the parasite Loa loa is also found. Treatment with ivermectin can be fatal for persons with a heavy burden of Loa loa infection; the combination of Strongyloides and Loa loa infection thus requires specialized treatment at dedicated centers.
This patient was from a country in which Strongyloides is endemic and he should have been screened for Strongyloides infection before any immunosuppressant medications (such as chemotherapy or steroids) were started. Since strongyloidiasis can last for life, ideally all persons at risk should be screened, but it is imperative to screen patients who are about to receive or who have recently started steroids or other immunosuppressive medications. All patients who are going to be treated with immunosuppressive drugs should be evaluated for risk factors and tested for strongyloidiasis; persons at risk should be treated empirically if immunosuppression needs to be initiated before the results of testing become available (e.g., for acute COVID-19). Thus, all providers, including primary care physicians, oncologists, rheumatologists and pulmonologists who frequently administer immune suppressive medications, should keep Strongyloides in mind and be proactive with appropriate testing.
Diagnostic Considerations
Although Strongyloides infects millions of people worldwide, screening is not common during normal immigration procedures, nor after individuals return from visits to countries where it may be endemic, and it is not routinely considered by U.S. physicians.5 Elevated eosinophil counts can be an important clue to a possible parasitic infection, but eosinophilia also occurs in many other conditions, such as infectious diarrhea, inflammatory bowel diseases and atopic conditions.6 Inflammatory bowel diseases can present with similar symptoms but are much more likely to have an associated finding of blood in the stool. Further testing to rule out inflammatory bowel disease requires colonoscopic examination and biopsy. There are also other eosinophilic gastrointestinal diseases (EGIDs) such as eosinophilic esophagitis and eosinophilic gastroenteritis, but these conditions usually present with upper gastrointestinal symptoms such as nausea, vomiting, and early satiety. Atopic conditions such as asthma can elevate eosinophil counts but are not commonly associated with diarrhea.2 Often, a white cell “differential” count is not automatically performed when a CBC (complete blood count) is ordered. However, in a patient with the appropriate social or travel history, screening for Strongyloides infection should include a CBC with “differential” and an antibody test, especially before initiation of any steroid or immunosuppressive medications.
In using the DEER taxonomy to better characterize what happened in the diagnostic process in this case, we can see that errors occurred in several aspects of the patient’s care – including in history taking, testing, and assessment. There was a “failure/delay in eliciting a critical piece of history data”; specifically, the repeated overlooking of his elevated eosinophil count which should have raised suspicion of a potential parasitic infection. Recognizing and following up on this abnormal test result in a timely manner could have prevented such a long delay in his diagnosis. In addition, in his numerous physician visits for diarrhea, there was failure to consider the diagnosis of a parasitic infection, failure to order indicated tests, and too much weight placed on competing explanations for his eosinophilia and diarrhea.6
System Considerations
Limited knowledge of parasitic helminths by US clinicians puts a large population of patients in iatrogenic danger.7 All clinicians, especially those in primary care, critical care, rheumatology, pulmonology, and oncology, should be aware of the importance of identifying patients who should be screened for Strongyloides infection based on their social and travel history. Clinicians who prescribe immunosuppressive medications should also know how to properly treat these patients before they receive corticosteroids or other medications that could put them at risk of hyper-infection. Building awareness among at-risk patients and families about strongyloidiasis and screening options, along with the availability of relatively safe and simple curative treatment, could also be helpful. Health departments can play a greater role in alerting clinicians and laboratories to the most recent epidemiological findings, to heighten clinical suspicion for strongyloidiasis and the capacity to treat.7 Clinician education can be supported by protocols or computerized reminders (e.g., triggered by an initial prednisone order for patients who have lived or extensively traveled in tropical and subtropical regions).But such computerized reminders need to be designed and implemented with sensitivity, to avoid adverse prejudicial or legal harms, given potential stigma and discrimination that can be associated with recent migration and/or chronic parasitic disease.8-10
Take-Home Points
- Strongyloides infection is common in tropical and subtropical regions and is not infrequently seen in immigrant and low-income communities in the US.8
- The social and travel history of patients is critical to identify who is at risk for this infection, especially when combined with unexplained GI symptoms or eosinophilia.
- Any patient who is being considered for treatment with steroidal or immunosuppressive medications and who is at risk of Strongyloides infection should be screened and treated, if necessary, before beginning those medications.
- Screening in the United States should be done with an antibody test on a blood sample.
- Eosinophilia can be a clue to underlying Strongyloides infection but clinicians should not be deterred by its absence. Likewise, a stool test for Strongyloides larvae is diagnostic if positive, but given its poor sensitivity, a negative result does not rule out infection. An antibody test is preferred.
- Ivermectin is a curative treatment for Strongyloides, but re-infection can occur if there is ongoing exposure.
- Strongyloides hyperinfection has a high mortality even with treatment. It should be completely preventable with appropriate screening. Diagnostic delays can significantly increase the risk of death.
Narath Carlile, MD, MPH
Department of Internal Medicine
Primary Care Research in Diagnostic Errors (PRIDE)
Brigham and Women’s Hospital
Harvard Medical School
Clyde Lanford Smith, MD, MPH, DTM&H
Department of Internal Medicine
Brigham and Women’s Hospital
Harvard University TH Chan School of Public Health
James H. Maguire, MD
Department of Internal Medicine, Division of Infectious Diseases
Brigham and Women’s Hospital
Harvard Medical School
Gordon D. Schiff, MD
Department of Internal Medicine
Associate Director, Center for Patient Safety Research and Practice
Primary Care Research in Diagnostic Errors (PRIDE)
Brigham and Women’s Hospital
Harvard Medical School
Acknowledgements:
The long-standing process for submitting PSNet WebM&M case submissions is anonymous. Users may contribute by submitting a case at the following link: https://psnet.ahrq.gov/webmm/submit-case
Periodically, the Primary-Care Research in Diagnosis Errors (PRIDE) Learning Network, a collaborative project convened by the Brigham and Women’s Hospital Center for Patient Safety Research and Practice, and the State of Massachusetts Betsy Lehman Center for Patient Safety, contributes cases and commentaries from their monthly discussions of diagnosis error cases to PSNet. PRIDE is funded by a grant from the Gordon and Betty Moore Foundation. This case was produced in cooperation with the PRIDE Learning Network. We acknowledge Sevan Dulgarian for editorial support in preparing this case discussion.
References
- Segarra-Newnham M. Manifestations, Diagnosis, and Treatment of Strongyloides stercoralis Infection. Ann Pharmacother. 2007;41(12):1992-2001. [Available at]
- Gonzales DJ, Chakraborty RK, Climaco A. Strongyloidiasis. [Updated 2022 Apr 22]. In: StatPearls [Internet]. [Free full text]
- Carnino L, Schwob JM, Gétaz L, et al. A practical approach to screening for Strongyloides stercoralis. Trop Med Infect Dis. 2021;6(4):203. [Free full text]
- Salvador F, Sulleiro E, Sánchez-Montalvá A, et al. Usefulness of Strongyloides stercoralis serology in the management of patients with eosinophilia. Am J Trop Med Hyg. 2014;90(5):830-834. [Free full text]
- Boulware DR, Stauffer WM, Hendel-Paterson BR, et al. Maltreatment of Strongyloides infection: case series and worldwide physicians-in-training survey. Am J Med. 2007;120(6):545.e1-545.e5458. [Free full text]
- Kuang FL. Approach to patients with eosinophilia. Med Clin North Am. 2020;104(1):1-14. [Free full text]
- Singer R, Xu TH, Herrera LNS, et al. Prevalence of intestinal parasites in a low-income Texas community. Am J Trop Med Hyg. 2020;102(6):1386-1395. [Free full text]
- Bushwick S. What causes prejudice against immigrants, and how can it be tamed. Sci Am July 2011;29:2011. [Free full text]
- Siteti M, Injete S, Wanyonyi W. Helminthiases: a neglected cause for reproductive ill-health and social stigma. Parasitologists United Journal 2015;8(2):87-94. (Review Article). [Free full text]
- Kane JC, Elafros MA, Murray SM, et al. A scoping review of health-related stigma outcomes for high-burden diseases in low- and middle-income countries. BMC Med. 2019;17(1):17. [Free full text]