Thin Air
Case Objectives
- Identify the gas-specific non-interchangeable connectors used for bulk gas supply outlets in hospitals.
- Define forcing function, both in engineered safety devices and in human procedures.
- Review strategies for prevention of delivery of wrong gas to hospitalized patients.
Case & Commentary: Part 1
A 73-year-old woman was admitted to the hospital with fever and back pain, and was diagnosed with pyelonephritis. The morning after admission, she became hypotensive and short of breath. Her oxygen saturations were 70%. She was placed on high-flow oxygen with little benefit. A chest x-ray showed diffuse pulmonary infiltrates consistent with acute respiratory distress syndrome (ARDS). The patient was intubated for type I (hypoxemic) respiratory failure, and placed on high flow oxygen. Shortly thereafter, the respiratory therapist arrived and noticed that the patient was being treated with compressed air—not oxygen.
In this case, it seems that both the high-flow oxygen mask and the self-inflating bag were hooked up to an air flowmeter, not an oxygen flowmeter. The hospital gas supply delivers gas under pressure to outlets in clinical settings.(1,2) In a ward room, or bay in the Emergency Department or ICU, these are typically on wall panels at the head of the bed. The working pressure for such outlets for both air and oxygen are about 45-55 PSI, a pressure too high to deliver directly to masks and bags. A flowmeter is connected to the outlet to meter gas at an appropriate flow rate, typically 1-15 liters per minute, at only slightly higher than ambient pressure. Such flowmeters are used to provide gas to bags, masks, nebulizers, and other simple ventilatory devices. More complex devices—like ventilators or anesthesia machines—have hoses carrying compressed gas attached directly to the compressed gas outlets.
The flowmeters used for air and oxygen are nearly identical, differing to the casual observer, if at all, only in the color-coding of the knobs or "Christmas Tree adapter," which provides a place to securely attach delivery tubing and other portions (Figure 1). Green adapters are meant for oxygen and yellow adapters are meant for air. Although the flowmeter itself may be physically designed to insert into only its specific gas port (see below), the threading for connection between the flowmeter and the Christmas tree adapter is universal in size. Thus, it is possible for an air flowmeter to have the green Christmas tree adapter attached instead of a yellow one (Figure 2). Someone attaching the delivery tubing might easily attach it to the green Christmas tree adapter, expecting it to be connected to the oxygen flowmeter and not noticing that it is actually an air flowmeter plugged into an air outlet. Even with the appropriate color Christmas tree adapter, it is quite possible to attach the tubing to the wrong flowmeter, especially in a crowded space under high stress and time pressure. Further, tubing from multiple airway devices may be attached to the various flowmeters simultaneously (eg, a self-inflating bag, a nebulizer, and a face mask), making recognition difficult.
How frequently such swaps occur is not known, but they do so often enough that on March 5, 2002 a Patient Safety Advisory on this topic was issued by the Veterans Health Administration Warning System. It is probably even more common for oxygen tubing to become disconnected from a correct flowmeter during a resuscitation. This issue is not easily recognized when a facemask or self-inflating bag is used, because these devices provide little feedback as to the gas flow rate.
Case & Commentary: Part 2
The patient was transferred to intensive care and died the next day of overwhelming sepsis and systemic inflammatory response syndrome (SIRS).
In this case, although errors occurred in providing supplemental oxygen, the patient's underlying disease was likely severe enough to cause death even in the absence of errors. Nonetheless, a typical response to such an event would be to blame clinicians for being ignorant, or lacking vigilance. However, employing human factors engineering concepts to this case would be more productive. In addition to avoiding a culture of blame and striving to identify root causes, the solutions offered by this approach rely on improving the design of artifacts in the world rather than relying on labels, instructions, training, or the usual admonition to "be more careful."(3)
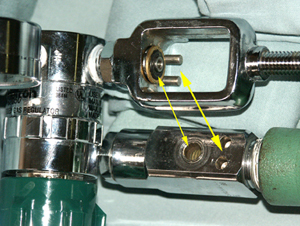
Much of the gas delivery system is designed to avoid hooking up the wrong gas hose to a compressed gas port through the use of physically non-interchangeable gas-specific connectors. While there are several such systems, perhaps the strongest is called the Diameter Index Safety System (DISS) (Figure 3). It is physically impossible to insert the oxygen hose or flowmeter into any other port, or to attach something inappropriate into the oxygen port. However, this safety net is incomplete. The threaded output of the flowmeter is "one size fits all" and fits yellow, green, and clear Christmas tree adapters. If some sort of diameter-indexed system were extended also to the flowmeter output port, or if the Christmas tree adapter was molded into the device, no crossover of the adapters could occur. That would solve the problem of the mismatched adapters, but it still would not prevent attachment of oxygen tubing to a non-oxygen flowmeter. A gas-specific non-interchangeable fitting for low-pressure oxygen tubing would be possible to produce, but is not currently a standard. Thus, the protection is not carried all the way to the end-user.
A physical arrangement that precludes doing the wrong thing, like the gas-specific non-interchangeable connector, is an example of an engineered safety device (ESD), and a forcing function.(3) Other forcing functions include "lockins," "lockouts," and "interlocks."(4) Lockins maintain a condition, and prevent easy exit from a sequence of actions until the right conditions are met. Lockouts prevent easy entrance to a dangerous set of actions or a segment of software, without the proper conditions and access authority. Interlocks enforce correct sequencing or isolate events in time; often they are used to prevent one action from being taken while another is already active. There are a variety of examples of these forcing functions in health care.(5)
In addition to the indexing system for connectors for bulk-supplied compressed gases, there is an indexing system for medical gas cylinders, called the "Pin Index System."(1,2) Each cylinder has a specific pattern of holes into which the matching pattern of pins from the appropriate regulator must fit (Figure 4). This helps to prevent the wrong regulator (in calibration and in color-code) from being attached to a cylinder. For example, I recently asked for an E-cylinder of oxygen to transport a critically ill patient, and the nurse complained that the regulator wouldn't fit on the tank properly. The nurse had inadvertently brought a CO2 cylinder (gray in color) instead of an oxygen cylinder. The Pin Index System prevented the oxygen regulator from being attached to the CO2 cylinder, perhaps saving the patient's life (since, once mounted under the bed, it would have been difficult to detect this error). Ventilation with 100% CO2 would rapidly cause a cardiac arrest in the patient, and the usual resuscitative measures of promoting a clear airway, adequate breathing, etc., would have only worsened matters (by promoting more exchange of the wrong gas) if the gas swap were not discovered.
Engineered safety devices and forcing functions are very common in anesthesiology, where experience has shown that good intentions, warnings, or vigilance are not sufficient to ensure patient safety. For example, the anesthesia machine itself has flowmeters to control the flow of oxygen, nitrous oxide, and air. In the heat of a crisis, or at the end of an anesthetic, the anesthesiologist might reach back to turn off the nitrous oxide and turn up the flow of oxygen, but inadvertently do exactly the opposite. Modern anesthesia machines contain a mechanical, pneumatic, or electronic oxygen proportion limiting control system that physically prevents selecting an oxygen concentration of less than 25%.(6-8) Another forcing function is the mechanical "vaporizer interlock" that prevents activating more than one vaporizer delivering a volatile anesthetic gas (eg, Isoflurane) at a time.(6-8)
Engineered safety devices and mechanical forcing functions are less common in the rest of medical practice. In radiation therapy or X-ray units, interlocks may prevent activating the radiation while the door to the unit is open. Most computer-based systems have forcing functions in software that double checks for irreversible actions (eg, "Do you really want to empty the trash?"). However, frequent users sometimes click this by habit even when they do not mean to approve the action.(4) This kind of behavior was a factor in a set of catastrophic errors with radiation therapy equipment.(9)
Despite effective forcing functions, near misses and errors may still occur. For example, in another case I asked for an oxygen cylinder, and was brought a CO2 cylinder with a CO2 regulator attached (these are used for certain purposes in cardiac surgery). The Pin Index System played no role here, since it forces the correct regulator on the matching tank and there was no mismatch in this case. There is no engineered safety device to ensure that the gas flowing is in fact oxygen. The anesthesia machine has alarms for oxygen concentration, but these are not yet used for in-hospital transport situations. Fortunately, I noticed the gray color (color-coding is another safety feature) of the tank.
There are also "procedural forcing functions" in which the standard procedures call for personnel to verify certain conditions before allowing actions to proceed. The requirement for a two-person check of blood products before administration to the patient is an example. The recently standardized "timeout" required by JCAHO and the VA before surgical incision is a procedural forcing function by which surgery cannot proceed unless all team members have re-verified the patient's identity, the proposed surgical procedure, and the exact site of surgery. Procedural forcing functions like this can be valuable if implemented systematically, and if the team is in fact empowered to act as an interlock. However, procedural forcing functions are relatively weak due to psychological factors such as haste, complacency, and a behavior termed "social shirking." Social shirking occurs when "members of an organization find it to their advantage to evade their work responsibilities and trust that the efforts of others are sufficient...to meet their goal."(10) When shirking is present, checks that are independently redundant in theory are neither independent nor redundant in practice.
What are potential specific solutions to the problem of mismatched adapters on flowmeters? One solution is to eliminate air flowmeters in most patient care settings. They appear to be used for two main purposes: to administer nebulized medications (eg, bronchodilators), and to provide humidified air to patients with a tracheostomy. Yet, nebulized medications can be delivered as safely using oxygen in all but a handful of cases. For those rare cases, either an air flowmeter or an air cylinder and flowmeter could be available. For patients with a tracheostomy, the humidified gas is usually administered via large bore tubing from a device that attaches directly to the flowmeter, without a Christmas tree adapter (Figure 5). Hence, many hospitals have banished air flowmeters with these adapters. Other sites have found this hard to do, because they argue that it requires more storage space and more effort to obtain the air devices in the cases where they are truly needed. The VA Advisory suggests converting color-coded Christmas tree adapters to clear ones (Figure 6) so that the adapter itself conveys no information as to the gas' identity, forcing the user to look at the flowmeter itself. This may not be a very effective way to alter the frequency of connecting the tubing to the wrong flowmeter.
Ultimately, indexing the tubing and fittings might be the better solution. In addition, following the lead of the anesthesia machine, developing oxygen analyzer systems for low-pressure oxygen delivery systems, allowing verification of oxygen concentration, would reduce errors related to gas administration.
Take-Home Points
- Examine the use of gas flowmeters in your institution and consider the various strategies to reduce the likelihood of connecting oxygen tubing to the wrong gas: - Eliminate air flowmeters; - Permanently fix Christmas tree adapters to the correct flowmeter; and - Use clear Christmas tree adapters rather than color-coded ones.
- Consider the possibility that the wrong gas (or no gas) is being administered when a patient does not respond to treatment with supplemental oxygen. Double check the flowmeter and tubing connections.
- Consider the use of forcing functions in other portions of the hospital. Look for possible design solutions wherever possible rather than relying solely on training, warnings, or labels.
David M. Gaba, MD Professor of Anesthesia Stanford University School of Medicine Staff Anesthesiologist VA Palo Alto Health Care System
Faculty Disclosure: Dr. Gaba has declared that neither he, nor any immediate member of his family, has a financial arrangement or other relationship with the manufacturers of any commercial products discussed in this continuing medical education activity. In addition, his commentary does not include information regarding investigational or off-label use of pharmaceutical products or medical devices.
References
1. Eichhorn J, Ehrenwerth J. Medical gases: storage and supply. In: Ehrenwerth J, Eisenkraft J, eds. Anesthesia equipment. St. Louis, Mo: Mosby; 1993.
2. Dorsch J, Dorsch S. Understanding anesthesia equipment. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 1999.
3. Norman D. The psychology of everyday things. New York, NY: Basic Books; 1988.
4. Leveson N. Safeware: system safety and computers. Reading, MA: Addison-Wesley Publishing Company; 1995.
5. Gosbee J. Human factors engineering and patient safety. Qual Saf Health Care. 2002;11:352-4.[ go to PubMed ]
6. Petty C. The anesthesia machine. New York, NY: Churchill Livingstone Inc.; 1987.
7. Eisenkraft J: The anesthesia machine. In: Ehrenwerth J, Eisenkraft J, eds. Anesthesia equipment. St. Louis, Mo: Mosby; 1993:27-56
8. Andrews J. Inhaled anesthetic delivery systems. In: Miller RD, ed. Anesthesia. 5th ed. New York, NY: Churchill Livingstone; 2000:174-206.
9. Leveson N. Medical devices: the Therac-25 story. In: Leveson N, ed. Safeware: system safety and computers. Reading, MA: Addison-Wesley Publishing Company; 1995:515-553.
10. Heimann C. Acceptable risks: politics, policy, and risky technologies. Ann Arbor, MI: The University of Michigan Press; 1997.
Figures
Figure 1. The air and oxygen flowmeters with the correct Christmas tree adapters.
Figure 2. The air and oxygen flowmeters with the Christmas tree adapters swapped.
Figure 3. The compressed gas outlets for oxygen and air illustrating the Diameter Index Safety System. The threaded connector for the oxygen outlet is much smaller than that needed for the air outlet, making it physically impossible to attach the oxygen hose to the air outlet.
Figure 4. Pin Index System on an oxygen cylinder. Photograph shows the pins on the regulator which fit in matching holes on the cylinder. Other gases have different pin positions.(1,2)
Figure 5. For tracheostomy, humidified gas is administered via large bore tubing from a device that attaches directly to the flowmeter, without a Christmas tree adapter.
Figure 6. An oxygen flowmeter with a clear Christmas tree adapter. If all flowmeters use this arrangement, it forces the user to look at the flowmeter itself or the wall outlet for color code information.