A Laceration that Needed a Proper Exam, Not an X-Ray
Wander J, Barnes DK. A Laceration that Needed a Proper Exam, Not an X-Ray.. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2024.
Wander J, Barnes DK. A Laceration that Needed a Proper Exam, Not an X-Ray.. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2024.
Debra Bakerjian, PhD, APRN, RN; David K. Barnes, MD; Patrick Romano, MD, MPH; Ulfat Shaikh, MD; Jazmin A. Wander, MD for this Spotlight Case and Commentary have disclosed no relevant financial relationships with ineligible companies related to this CME activity.
Learning Objectives
At the conclusion of this educational activity, participants should be able to:
- Perform a neurovascular and functional hand examination.
- Recognize the risk of occult hand tendon injuries.
- Describe the various human factors that contribute to missed hand injuries.
- Suggest possible approaches to mitigating errors caused by human factors.
The Case
A healthy 57-year-old right hand dominant woman presented to the emergency department (ED) for evaluation of a laceration to the palmar aspect of her left thumb. Hours before presentation, she accidentally cut herself with a kitchen knife. The treating clinician documented a superficial 3cm laceration and that the patient was unable to flex her thumb due to pain. Neither a sensory examination nor wound exploration was documented. No fracture or foreign body was identified on x-ray. The clinician closed the laceration with sutures. A splint was not applied. The absence of a foreign body was documented in the procedure note but not whether the tendon was visualized. The patient was discharged from the ED and follow-up was arranged with her primary care physician (PCP). She was still unable to flex her thumb at follow-up a few weeks later. She was referred to an orthopedic surgeon who referred her to a hand specialist who surgically repaired her left thumb flexor tendon laceration. Despite repair, her left thumb function remained significantly limited.
The Commentary
By Jazmin A. Wander, MD, and David K. Barnes, MD, FACEP
In this case, the failure to perform a complete hand examination and appropriately manage and refer a high-risk laceration led to the delayed diagnosis of a thumb flexor tendon laceration and subsequent functional impairment. The clinician’s documentation suggests their hand examination was incomplete. Moreover, because the injured digit was not splinted, it appears that the risk to the underlying tendon was not fully appreciated. Even under ideal circumstances, it may be difficult to visualize a lacerated flexor tendon given the deep anatomic location of these structures. Many hand tendon lacerations are occult; confirmation requires advanced imaging or definitive surgical exploration. Nevertheless, physical examination clues—in particular, the inability to flex the injured digit, and significant pain with active range of motion—should have alerted clinicians in this case to the possibility of a complete or partial tendon laceration.
Background
The hand is a highly specialized anatomic unit. Its function is facilitated by an intricate network of tendons that enable essential movements of the fingers, thumb, and wrist. Hand injuries are one of the most common emergency department (ED) chief complaints. In the United States, an estimated 2.6 million annual ED visits are attributed to hand and wrist injuries.1 From 2009 to 2012, hand-related complaints accounted for over $180 billion in healthcare expenditures.2 Extensor and flexor tendons may be injured due to penetrating trauma (i.e., open lacerations) or because of exaggerated biomechanical forces (i.e., closed ruptures).
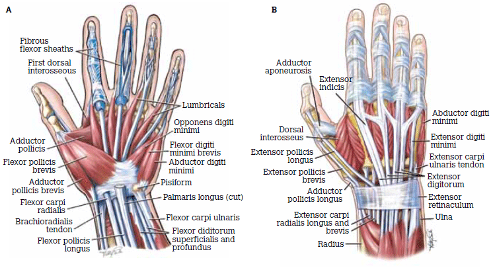
Figure 1. Tendons and Muscles of the Wrist, Hand and Fingers
Source: Grant, John Charles Boileau, Public domain, via Wikimedia Commons
Extensor tendons originate from muscles in the posterior compartment of the forearm, particularly the extensor digitorum (ED) and extensor indicis (EI) muscles, and are found along the dorsum of the wrist, hand, and fingers (Figure 1). These tendons are relatively superficial to the skin surface making them more susceptible to injury than flexor tendons. They insert directly onto the dorsal surfaces of the phalanges and provide counteracting forces to extend the digits.
Flexor tendons are located on the voar (i.e., palmar) aspect of the wrist, hand, and fingers and originate from the flexor digitorum profundus (FDP), flexor digitorum superficialis (FDS), and flexor pollicis longus (FPL) muscles located in the anterior compartment of the forearm (Figure 1). Flexor tendons lie deeper within the hand compared to extensor tendons and are dependent upon an elaborate annular and cruciate pulley system that multiplies mechanical forces, reduces friction, and prevents bowstringing during flexion. Flexor tendons are more difficult to visualize during wound exploration.3
Approach to Patient Safety
Failure to perform a thorough hand examination can lead to missed open or closed tendon injuries often resulting in serious morbidity. Outcomes are worse when the diagnosis is delayed or missed altogether. Therefore, clinicians who evaluate hand injuries must maintain a high index of suspicion and have a low threshold to splint and refer patients for follow-up examination with a specialist if a tendon injury cannot be definitively excluded.
While complete tendon disruptions are usually clinically obvious, the anatomic location, physical structure, and in some cases redundancy of tendons may allow for movement of the affected digit even when the tendon is completely transected. Partial tendon lacerations may elude diagnosis if function remains intact. In a study of 165 patients undergoing wound exploration after hand laceration, 32% of tendon injuries were initially not diagnosed by either the ED clinician or the hand surgeon. This finding highlights the difficulty inherent to diagnosing such injuries and emphasizes the importance of appropriate follow-up in cases of suspected occult tendon injuries.4
Hand Examination
A thorough hand examination, including functional testing and neurovascular assessment, should be performed after an injury. The exam begins with external inspection. Underlying structures shift and move depending on the position of the hand, therefore, examine the wound with the hand in the same position as it was during the injury. Wounds should be evaluated for active bleeding, and perfusion to the injured area should be assessed by capillary refill. Explore wounds for evidence of arterial bleeding, foreign body, tendon injury, and arthrotomy.
Liberal use of local or regional anesthesia facilitates adequate exploration. Digital or regional nerve blocks improve patient comfort and allow the examiner to adequately assess a wound to its base. While the use of epinephrine in local anesthetics was previously believed to cause digital ischemia, its use is now considered safe and highly effective at prolonging anesthesia and arresting bleeding, thereby improving tissue visualization.5,6 Topical anesthetics can relieve some of the discomfort associated with local anesthetic infiltration, but systemic analgesia and anxiolysis may be required in some cases.
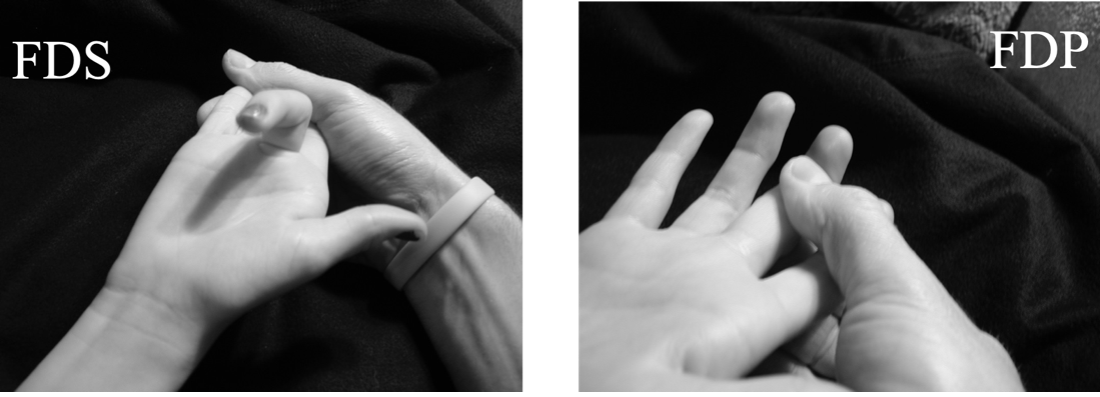
Figure 2. Testing Flexor and Extensor Tendons
Source: Courtesy of David K. Barnes, MD (commentary author).
Clockwise from top left: FDS (flexor digitorum superficialis); FDP (flexor digitorum profundus); EDI (extensor digiti indicis); EDC (extensor digitorum communis).
The functional exam includes assessment of motor function, sensation, range of motion, and tendon integrity. Sensation should be assessed by two-point discrimination. Carefully test both active and passive range of motion at the metacarpophalangeal, proximal interphalangeal, and distal interphalangeal joints. Because tendons impart different movements depending on the phalanx or joint assessed, each tendon must be tested independently (Figure 2). Extensor tendon disruption is obvious when a digit lies in passive flexion and cannot be extended. Conversely, flexor tendon disruption is obvious when the digit rests in passive extension and cannot be flexed. Importantly, movement is still possible even when 95% of the tendon cross section is disrupted, especially with flexor tendons.7 Therefore, if there is pain or weakness with active range of motion and movement against resistance, one should assume that a partial tendon disruption is present.8
Patient factors can limit the quality and completeness of the hand examination. Barriers to a complete hand exam include pain, anxiety, intoxication, limb- or life-threatening injuries, or language/communication barriers. Cooperation with range of motion testing is a key component of functional testing. Patients should lie supine during the exam to avoid vasovagal reactions that could lead to falls and new injuries. A well-lighted and bloodless surgical field is essential. For digital lacerations, finger tourniquets are commercially available, but a cut sterile glove or standard phlebotomy tourniquet secured with hemostats are simple and effective alternatives. A blood pressure cuff applied proximal to the wound is another option. Because of their shallow location, extensor tendons are relatively easy to identify and inspect. Flexor tendons lie deep and are more difficult—and sometimes impossible—to visualize. However, it is not essential to directly visualize a flexor tendon laceration, or any tendon laceration for that matter, during the initial ED evaluation. Indirect evidence of injury based on functional testing is sufficient to suggest a tendon injury, and conservative splinting and referral should follow accordingly.8
Clear and complete documentation of the hand examination ensures accurate communication, continuity of care, and a legal record of the clinician’s assessment in case of future quality or medical-legal concerns.
Imaging
Imaging is routine for most hand injuries but is not necessary for all hand lacerations. Diagnostic radiography can assess for underlying fractures or the presence of radiopaque foreign bodies such as teeth, glass, or metal. Imaging may reveal evidence of traumatic arthrotomy by demonstrating air in the joint space. Diagnostic radiographs should not be used to rule in or rule out a tendon laceration.
Point of care ultrasound can be used to assess for open or closed tendon injuries and is a useful adjunct to the clinical examination. Ultrasound offers real-time, high-resolution visualization of soft tissues and can identify tendon injuries, characterize their location and severity, and guide decisions regarding surgical intervention. Some studies suggest ultrasound is faster than traditional wound exploration, magnetic resonance imaging (MRI), or surgical consultation, and more accurate than physical examination alone.9 The quality of sonographic imaging is highly operator dependent.10 Therefore, wound exploration remains the standard of care.
Tendon Injury Management
A complete discussion of the treatment of hand tendon lacerations is beyond the scope of this commentary. However, there are several important management considerations that will improve patient safety and functional outcomes.
Hand and wrist tendons may be repaired in the ED or later in the ambulatory setting. Most tendon injuries should be repaired by an experienced hand surgeon; however, some tendon injuries may be repaired by a qualified and experienced emergency clinician. The choice between primary (immediate or near term) and secondary (delayed) repair depends on the location and extent of the injury, the clinical setting (e.g., academic versus rural hospital), and the operator’s experience and ability.11,12
Emergency physicians may attempt to repair extensor tendon injuries over the proximal phalanx and metacarpals, but it is not mandatory that they do so. If repair is attempted, discussion with a hand surgeon is advised. Unless there is concern for infection or an open fracture, it is perfectly acceptable to provide wound care (i.e., copious irrigation, exploration, skin closure, and tetanus and antibiotic prophylaxis, if indicated), splint the injury, and refer patients for specialty follow-up.8,11
Flexor tendon lacerations should only be repaired by a hand surgeon. Many patients undergo primary repair, although those who undergo secondary repair have similar outcomes.13
Whether or not tendon repair is attempted in the ED, the hand and wrist should be splinted to stabilize the injury, prevent tendon retraction (which may make surgical repair more challenging or impossible), and ensure optimal healing and functional recovery. Close follow-up with a hand surgeon should be arranged for all cases of definite or suspected tendon disruption.8
Referral and Follow-up
Depending on local practice patterns and consultant availability, it may be appropriate to consult a hand surgeon from the ED or to urgently refer patients for follow-up outpatient evaluation. Referred patients should ideally be seen within 5 days, though this is not always possible. In cases of definite tendon disruption, specialty follow-up ensures timely management, including operative treatment. Specialists are more skilled at evaluating patients with suspected occult tendon injuries and may refer them for advanced imaging (e.g., MRI) or surgical exploration. Timely specialty consultation and prompt follow-up contribute significantly to optimizing patient outcomes, reducing the risk of complications, and restoring hand function.
Human Error
As this case illustrates, human error is a common cause contributing to poor outcomes after hand trauma. In a retrospective study of legal claims of negligence for hand and upper extremity surgery in Greece, misdiagnosis was the most common claim. The authors attributed misdiagnosis primarily to a lack of knowledge, lack of experience (including examination by a trainee), and lack of injury pattern recognition. Distracting injuries and poor patient compliance also contributed.14
In another study of 500 consecutive patients with hand injuries in Northern Ireland referred to a plastic surgery unit, the initial treating clinicians—including both emergency physicians and hand surgeons—missed 16 (3.2%) injuries, most (11/16, 69%) involving tendons. The authors attributed misdiagnosis primarily to failure to perform a comprehensive hand examination. Additionally, most of the missed injuries involved glass and examination by a trainee, but both examiner inexperience and lack of knowledge factored substantially. These authors noted several opportunities to reduce the incidence of missed tendon injuries including next day specialist clinic follow-up, completion of a thorough history, performance of a comprehensive hand examination, and the use of a hand chart to document injuries accurately.15
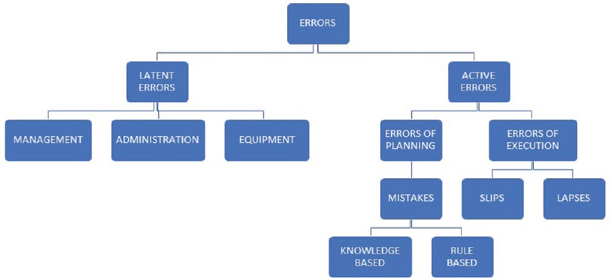
Figure 3. Sources of error in healthcare
Source: Sameera V, Bindra A, Rath GP. Human errors and their prevention in healthcare. J Anaesthesiol Clin Pharmacol. 2021;37(3):328-335.
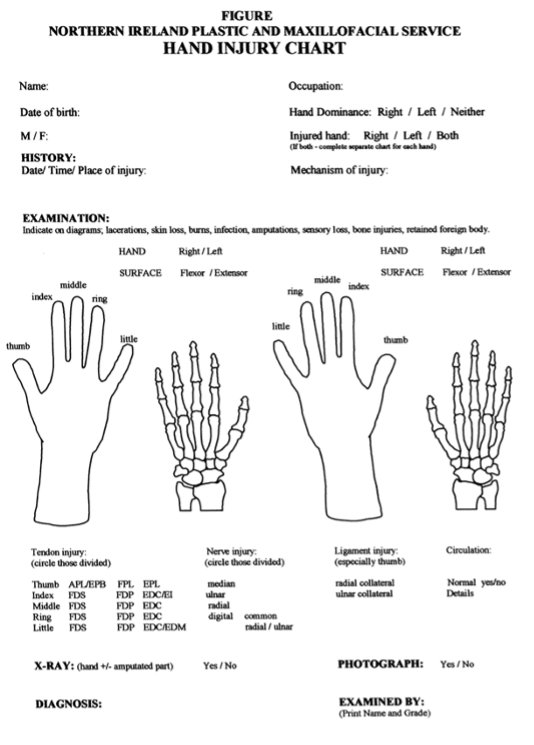
Slips and lapses are common sources of medical error involving task execution. Knowledge- and rules-based mistakes comprise the remainder of active human errors (Figure 3). A lapse is an error that occurs pursuant to erroneous memory. In this case, the examiner may have simply forgotten to check the integrity of the tendon or to explore to the base of the wound. Lapses may be overcome by relying less on memory and instead employing cognitive aids such as algorithms, checklists, and visual aids.16 While a checklist or visual aid is never a substitute for adequate training and experience, a hand chart, like that used by the Ulster Clinic in Northern Ireland (Figure 4), if embedded into the medical record and used contemporaneously with the exam, could serve as a reminder to clinicians about relevant anatomy and prompt a search for specific injuries.15
Figure 4. Example tool for assessing and evaluating hand injuries
Source: Morrison CM, Thompson NW, Herbert KJ, Brennen MD. Missed injuries in the acutely traumatised hand. Ulster Med J. 2003;72(1):22-25.
Slips occur because of erroneous performance of a required task. It is possible that the examiner in this case would have performed a complete hand examination under different circumstances. Slips due to fatigue, noise, or other distractions may lead a clinician to omit an essential task because the working environment is not optimal. Optimizing working conditions is critical to patient safety, and in this case may include adequate clinician rest, sufficient lighting, patient comfort and cooperation, and eliminating distractions which could disrupt the examination.16 It is not clear if the working environment contributed to this error.
Mistakes are errors in planning and can be attributed to gaps in knowledge, lack of skill and/or training, and various cognitive biases. One such bias is fixation, also known as anchoring. This occurs when a clinician favors a single diagnosis and is unable or unwilling to consider alternatives. The failure to splint this high-risk injury despite examination findings highly indicative of a flexor tendon laceration (i.e., inability to flex the thumb) suggests that the clinician lacked sufficient experience and training to evaluate and manage a complex hand injury. It also suggests the possibility they anchored on the laceration and failed to consider alternate diagnoses like deeper soft tissue injuries. Solutions to avoid mistakes include additional training, simulation, use of cognitive aids, and the use of cognitive forcing strategies.16 One example of a cognitive forcing strategy is found in our electronic health record which provides options to document specific injuries in the hand section of the physical exam. While not mandatory, users are prompted to consider abnormal findings (e.g., foreign body, tendon injury, arthrotomy, etc.) that may otherwise escape memory.
Take-Home Points
- Missed hand tendon injuries may lead to a poor functional outcome.
- A thorough hand examination, including neurovascular and functional testing, is required for all hand injuries.
- X-rays cannot be used to diagnose tendon injuries. Ultrasound is a useful adjunct when assessing for a tendon injury but is operator dependent. Neither test should replace a thorough hand exam and wound exploration.
- Unless infection or an open fracture is present, hand wounds should be managed with copious irrigation, exploration, skin closure, and if indicated, tetanus and antibiotic prophylaxis.
- If a tendon injury cannot be ruled out after wound exploration and functional testing, assume an occult injury exists. Specialty follow-up with a hand surgeon can ensure definitive diagnosis and treatment.
- Splint all cases of confirmed and suspected tendon injuries.
- Slips, lapses, and mistakes are common sources of human error. Additional training, cognitive forcing, checklists and visual aids, and awareness of cognitive biases are strategies to avoid human error.
Jazmin A. Wander, MD
Captain, USAF, MC
Resident Physician
Department of Emergency Medicine
UC Davis Health
jazwhite@ucdavis.edu
David K. Barnes, MD, FACEP
Consulting Editor, AHRQ, Patient Safety Network
Health Sciences Clinical Professor
Director of Faculty Development
Director of ED Sustainability
Department of Emergency Medicine
Physician Advisor
UC Davis Health
dbarnes@ucdavis.edu
References
- Gordon AM, Malik AT, Goyal KS. Trends of hand injuries presenting to US emergency departments: A 10-year national analysis. Am J Emerg Med. 2021;50:466-471. [Available at]
- Colen DL, Fox JP, Chang B, et al. Burden of hand maladies in US emergency departments. HAND. 2018;13(2):228-236. [Free full text]
- Jong JP de, Nguyen JT, Sonnema AJM, et al. The incidence of acute traumatic tendon injuries in the hand and wrist: a 10-year population-based study. Clin Orthop Surg. 2013;6(2):196-202. [Free full text]
- Nassab R, Kok K, Constantinides J, et al. The diagnostic accuracy of clinical examination in hand lacerations. Int J Surg. 2007;5(2):105-108. [Free full text]
- Lalonde D, Bell M, Benoit P, et al. A Multicenter prospective study of 3,110 consecutive cases of elective epinephrine use in the fingers and hand: the Dalhousie Project clinical phase. J Hand Surg. 2005;30(5):1061-1067. [Available at]
- Ilicki J. Safety of epinephrine in digital nerve blocks: a literature review. J Emerg Med. 2015;49(5):799-809. [Available at]
- Lineberry KD, Shue S, Chepla KJ. The management of partial zone II intrasynovial flexor tendon lacerations: a literature review of biomechanics, clinical outcomes, and complicatoins. Plast Reconstr Surg. 2018;141(5):1165-1170. [Available at]
- Sokolove PE, Barnes DK. Extensor and flexor tendon injuries in the hand, wrist, and foot. In: Roberts JR, Hedges JR, eds. Clinical Procedures in Emergency Medicine. 7th ed. Saunders Elsevier; 2019:956-979.
- Wu TS, Roque PJ, Green J, et al. Bedside ultrasound evaluation of tendon injuries. Am J Emerg Med. 2012;30(8):1617-1621. [Available at]
- Del Baño-Aledo ME, Martínez-Payá JJ, Ríos-Díaz J, et al. Ultrasound measures of tendon thickness: intra-rater, inter-rater and inter-machine reliability. Muscle Ligaments Tendons J. 2019;07(01):192. [Free full text]
- Sasor SE, Chung KC. Surgical considerations for flexor tendon repair timing and choice of repair technique and rehabilitation. Hand Clin. 2023;39(2):151-163. [Available at]
- Tang JB. Flexor tendon injuries. Clin Plast Surg. 2019;46(3):295-306. [Available at]
- Tang JB, Lalonde D, Harhaus L, et al. Flexor tendon repair: recent changes and current methods. J Hand Surg (Eur Vol). 2021;47(1):31-39. [Free full text]
- Vasdeki D, Varitimidis SE, Chryssanthakis C, et al. Medico-legal risks associated to hand and wrist trauma. World J Crit Care Med. 2022;11(1):40-47. [Free full text]
- Morrison CM, Thompson NW, Herbert KJ, et al. Missed injuries in the acutely traumatised hand. Ulst Méd J. 2003;72(1):22-25. [Free full text]
- Sameera V, Bindra A, Rath GP. Human errors and their prevention in healthcare. J Anaesthesiol, Clin Pharmacol. 2021;37(3):328-335. [Free full text]