Crossing the Line
Case Objectives
- Review complications of central venous catheterization
- Discuss patient and operator factors that affect complication rates
- Describe methods for preventing complications and for promptly identifying complications when they occur
Case & Commentary: Part 1
A 46-year-old man was admitted with pneumonia and confusion. The patient underwent an extensive work-up including bronchoscopy, which revealed a pyogenic lung abscess, and an MRI of the brain, which showed multiple ring-enhancing lesions. Intravenous (IV) antibiotic therapy was initiated. Due to poor peripheral IV access, a central venous catheter (CVC) was inserted by the attending physician. The procedure was performed at the right internal jugular site. At the end of the procedure, the operating physician reported excessive bleeding from the catheter site, but this was eventually controlled by manual pressure over the site. A chest radiograph was obtained after the procedure, and a radiologist interpreted the film as showing the catheter lying in the distal right jugular vein.
Central venous catheterization can result in mechanical, infectious, and thrombotic complications.(1) Mechanical complications, such as bleeding, hematoma formation, pneumothorax, and arterial puncture and cannulation, typically occur at the time of insertion (Table 1). Bleeding complications occur more commonly in patients with coagulation abnormalities or elevated central venous pressure.
Central venous catheterization can be performed at the internal jugular, subclavian, or femoral venous sites. Femoral venous catheterization should be avoided except in emergencies because it is associated with an increased risk of infectious and thrombotic complications.(2-4) The subclavian vein is the preferred site, especially in patients with indistinct landmarks for internal jugular catheterization. The subclavian site has the lowest rates of infection, thrombosis, and arterial puncture.(2-6) There is no difference in the rates of pneumothorax for internal jugular versus subclavian vein placement.(6) However, it is more difficult to control excessive bleeding when it occurs at the subclavian site. Importantly, patients generally find subclavian catheters more comfortable than the internal jugular catheters.
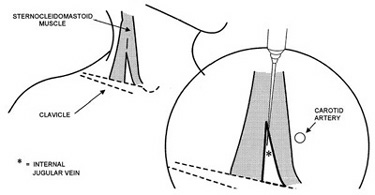
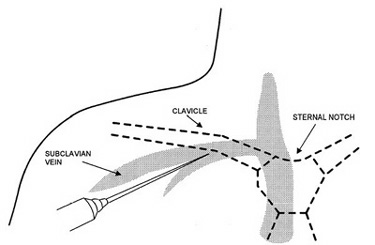
The internal jugular vein usually runs just lateral to the carotid artery as it traverses the anterior triangle formed by the sternocleidomastoid muscles (Figure 1). However, this relationship is not present in 20% of individuals, in whom the internal jugular vein may lie medial, deep, or just superficial to the carotid artery.(7) In contrast to the variable anatomy of the internal jugular vein, the anatomy at the subclavian site is more constant. The subclavian vein begins at the lateral border of the first rib and joins the internal jugular vein medial to the anterior scalene muscle to form the brachiocephalic vein (Figure 2). Throughout its course, it runs anterior and inferior to the artery. The junction of the middle and lateral thirds of the clavicle provides a useful surface landmark.
Several factors increase the risk of mechanical complications during CVC insertion. These can be divided into patient factors and operator factors. Patient factors include extremes of weight, prior surgery in the area of the site, prior catheterization at the same location, skeletal deformities (severe scoliosis, upper extremity or neck contractures), and inability to cooperate.(8) Perhaps the most important operator-related factor is experience. Physicians who have performed more than 50 catheterizations have half as many complications as less experienced operators.(3) Having three or more unsuccessful passes with the needle is also associated with increased complications.(8) Whenever possible, subsequent attempts should be made by a more experienced operator, or at a different site.
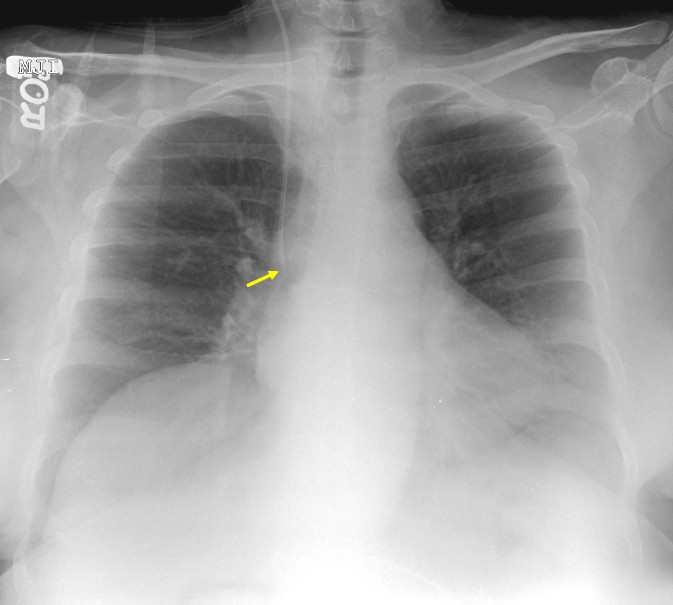
Post-procedure chest x-rays are used to confirm correct positioning of the catheter and to identify complications, such as hemothorax and pneumothorax. In general, radiographic confirmation of catheter location is reliable. When correctly positioned, the tip of the catheter lies at the cavo-atrial junction, at the level of the right mainstem bronchus (Figure 3). However, if a catheter is not inserted far enough, then the course of the venous and arterial system can be difficult to distinguish, which was probably the situation in this case (Figure 4). The suspected tip location suggests that at least 10 cm of the catheter was outside the patient's body, since most central venous catheters are 15-20 cm long. Conversely, if the catheter is inserted too far and enters the right atrium or right ventricle, arrhythmias or, less commonly, perforation of the myocardium can occur.
Case & Commentary: Part 2
Twelve hours after the procedure, the patient developed new dysarthria, dysphagia, and left hemiplegia. A repeat brain MRI showed new cerebral infarctions in the right frontal, parietal, and temporal lobes. A carotid ultrasound was obtained to rule out carotid stenosis. There was no evidence of carotid artery stenosis; however, the ultrasound showed that the CVC was within the lumen of the right carotid artery. The catheter was immediately removed. The patient suffered permanent neurologic deficits, including left hemiplegia. He was eventually discharged to a long-term skilled nursing facility.
Neurologic deficits following catheterization at the internal jugular site, similar to the ones seen in this case, suggest arterial injury or paradoxical embolization of thrombus or air through a right to left shunt. The timing of this patient's neurologic deterioration favors an arterial injury. An air embolism would be expected to result in immediate symptoms during insertion (or withdrawal), and catheter-related thrombosis often develops after a period of time.
Arterial puncture occurs in approximately 5% to 10% of internal jugular catheterization attempts.(3,9) Although pulsatile bright red blood is typically encountered when arterial puncture occurs (hitting "Big Red"), this finding can be unreliable. For example, volume overloaded patients breathing 100% oxygen can have pulsatile venous blood that appears quite red, and patients who are hypotensive and/or hypoxemic may have minimally pulsatile arterial blood that is surprisingly dark.
The key to preventing serious injury to the artery is identifying the arterial puncture prior to dilating the vessel. The ideal technique should be quick, easy to perform, and inexpensive. The most definitive technique is to attach a pressure transducer to the needle and inspect the waveform. Alternatively, one can insert a single lumen catheter without dilating the vessel and attach the transducer to the catheter. Venous waves are easily distinguished from arterial waves. Another option is to construct a manometer with a 20-cm to 30-cm piece of sterile IV tubing flushed with saline. After vessel cannulation, the tubing is attached to the needle and held upright. Arterial puncture is easily identified, as the saline column will not drop and blood will pulsate through the top of the tubing. In contrast, venous cannulation results in an immediate drop in the column of saline. Sending a venous blood sample for gas analysis is another option. Although this method often works, the result may be difficult to interpret if the patient is particularly well oxygenated or if hypercarbia is present. Simultaneous analysis of radial artery blood improves the accuracy of this technique. The major drawback to blood gas analysis is time delay, which can be minimized when point-of-care testing is available. In the event that the carotid or subclavian artery is dilated, vascular surgical consultation may be indicated. This is particularly important if a large catheter, such as an introducer sheath or a dialysis catheter, has been placed in an artery.
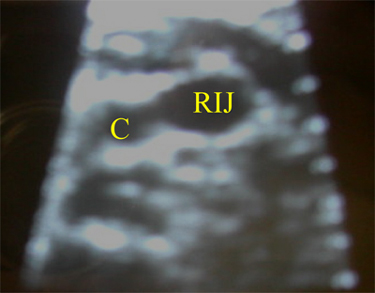
Using real-time ultrasound to guide internal jugular vein cannulation reduces complications and increases success rates.(10,11) In one study, the success rate with ultrasound guidance was 100%, compared with 88% when ultrasound was not used. The same study showed that the incidence of carotid puncture was reduced from 8.3% to 1.7%, and the average access time was reduced by a factor of four.(12) By using this aid, the internal jugular vein is easily identified (Figure 5) even in patients with thick necks and poorly visible landmarks. In contrast, visualizing the subclavian vein with ultrasound is more difficult; it is probably for this reason that the use of ultrasound for subclavian placement does not clearly reduce the incidence of complications.(8) The lack of clear benefit at the subclavian site may also be due to the more consistent anatomic relationship between the subclavian vein and surface landmarks.
Several inexpensive portable ultrasound machines are available for use (Figure 6). As with all new technologies, training is required to ensure optimal results. To avoid contamination of the site, specially designed sterile sleeves should be used to cover the transducer. Sterile gloves are not an appropriate alternative, because they do not cover the entire apparatus.
Mechanical, infectious and thrombotic complications of central venous catheterization are common but preventable. Reduction in mechanical complications can be achieved by ensuring adequate training and experience of the operator, preferential use of the subclavian site for vascular access, regular use of an ultrasound device to identify the target vessel when the internal jugular approach is necessary, and optimization of patient positioning prior to procedure. Table 2 lists several additional system-level interventions that may reduce the incidence of CVC-related complications.
To implement these changes with the greatest chances of success, health care systems should: (i) make it an institutional priority to reduce complications of central venous catheterization, (ii) identify a respected clinician to be an advocate for change, (iii) offer training courses in central line placement, (iv) ensure that necessary supplies (sterile drapes, portable ultrasound devices, chlorhexidine antiseptic solution, antibiotic-impregnated catheters) are readily available, (v) empower nurses to intervene when sterile precautions are not followed, and (vi) provide specific feedback to providers with high complication rates. Because brief, one-time interventions are not likely to result in lasting improvements, ongoing efforts to change both the attitudes and behaviors of providers are necessary.
Jeremy P. Feldman, MD E-Bay Fellow in Pulmonary Vascular Disease Stanford University School of Medicine
Michael K. Gould, MD, MS Research Associate and Staff Physician, VA Palo Alto Health Care System Assistant Professor of Medicine and of Health Research and Policy Fellow, Center for Primary Care and Outcomes Research Stanford University School of Medicine
Dr. Gould is supported by an Advanced Research Career Development Award from the Department of Veterans Affairs Health Services Research and Development Service. The views expressed in this commentary are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Faculty Disclosure: Drs. Feldman and Gould have declared that neither they, nor any immediate member of their family, have a financial arrangement or other relationship with the manufacturers of any commercial products discussed in this continuing medical education activity. In addition, their commentary does not include information regarding investigational or off-label use of pharmaceutical products or medical devices.
References
1. McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med. 2003;348:1123-33.[ go to PubMed ]
2. Merrer J, De Jonghe B, Golliot F, et al. Complications of femoral and subclavian venous catheterization in critically ill patients: a randomized controlled trial. JAMA. 2001;286:700-7.[ go to PubMed ]
3. Sznajder JI, Zveibil FR, Bitterman H, Weiner P, Bursztein S. Central vein catheterization: failure and complication rates by three percutaneous approaches. Arch Intern Med. 1986;146:259-61.[ go to PubMed ]
4. Durbec O, Viviand X, Potie F, Vialet R, Albanese J, Martin C. A prospective evaluation of the use of femoral venous catheters in critically ill adults. Crit Care Med. 1997;25:1986-9.[ go to PubMed ]
5. McKinley S, Mackenzie A, Finfer S, Ward R, Penfold J. Incidence and predictors of central venous catheter related infection in intensive care patients. Anaesth Intensive Care. 1999;27:164-9.[ go to PubMed ]
6. Ruesch S, Walder B, Tramer M. Complications of Central Venous Catheters: Internal Jugular versus Subclavian access-A Systematic Review. Crit Care Med. 2002;30:454-60.[ go to PubMed ]
7. Dickinson CS, Roth SM, Russell JM, et al. Placement of internal jugular vein central venous catheters: anatomic ultrasound assessment and literature review. Surg Rounds. 1996;19:102-16
8. Mansfield PF, Hohn DC, Fornage BD, Gregurich MA, Ota DM. Complications and failures of subclavian-vein catheterization. N Engl J Med. 1994;331:1735-8.[ go to PubMed ]
9. Martin C, Eon B, Auffray JP, Saux P, Gouin F. Axillary or internal jugular central venous catheterization. Crit Care Med. 1990;18:400-2.[ go to PubMed ]
10. Teichgraber UK, Benter T, Gebel M, Manns MP. A sonographically guided technique for central venous access. AJR Am J Roentgenol. 1997;169:731-3.[ go to PubMed ]
11. Randolph AG, Cook DJ, Gonzales CA, Pribble CG. Ultrasound guidance for placement of central venous catheters: a meta-analysis of the literature. Crit Care Med. 1996;24:2053-8.[ go to PubMed ]
12. Denys BG, Uretsky BF, Reddy PS. Ultrasound-assisted cannulation of the internal jugular vein. A prospective comparison to the external landmark-guided technique. Circulation. 1993 May;87:1557-62.[ go to PubMed ]
13. Raad II, Hohn DC, Gilbreath BJ, et al. Prevention of central venous catheter-related infections by using maximal sterile barrier precautions during insertion. Infect Control Hosp Epidemiol. 1994;15:231-8.[ go to PubMed ]
14. Maki DG, Stolz SM, Wheeler S, Mermel LA. Prevention of central venous catheter-related bloodstream infection by use of an antiseptic-impregnated catheter: a randomized, controlled trial. Ann Intern Med. 1997;127:257-66.[ go to PubMed ]
15. Veenstra DL, Saint S, Sullivan SD. Cost-effectiveness of antiseptic-impregnated central venous catheters for the prevention of catheter-related bloodstream infection. JAMA. 1999;282:554-60.[ go to PubMed ]
Tables
Table 1. Frequency of Mechanical Complications, According to the Route of Catheterization
| Complication | Frequency | ||
|---|---|---|---|
|
| Internal Jugular (%) | Subclavian (%) | Femoral (%) |
| Arterial puncture | 6.3 to 9.4 | 3.1 to 4.9 | 9.0 to 15.0 |
| Hematoma |
| 1.2 to 2.1 | 3.8 to 4.4 |
| Hemothorax | NA | 0.4 to 0.6 | NA |
| Pneumothorax |
| 1.5 to 3.1 | NA |
| Total | 6.3 to 11.8 | 6.2 to 10.7 | 12.8 to 19.4 |
Adapted from reference 1. NA= not applicable.
Table 2. Interventions that May Reduce the Risk of Complications
| 1. Limit catheter insertion to experienced operators (3) |
| 2. Consider peripherally inserted central venous catheters (PICC) when possible |
| 3. Have available ultrasound machines with a supply of sterile sleeves (10,11) |
| 4. Tape sterile IV tubing to the catheter kit |
| 5. Preferentially use the subclavian site (2-5) |
| 6. Optimize patient positioning prior to beginning the procedure (Trendelenburg for internal jugular insertions; towel roll under the back for insertion at the subclavian site) |
| 7. Use maximal sterile barrier precautions (large sterile drape, cap, gown, gloves, mask) (13) |
| 8. Use chlorhexidine solution to prepare the catheterization site |
| 9. Consider using an antibiotic impregnated catheter, especially if the institutional risk of infectious complications is above average (14,15) |
| 10. Assess ongoing need for central catheter at least once daily and promptly remove when no longer necessary |
Figures
Figure 1. Landmarks for Internal Jugular Approach
Figure 2. Landmarks for Subclavian Approach
Figure 3. Chest X-Ray Showing Catheter in Correct Position with Tip at Cavo-Atrial Junction
Figure 4. Chest X-Ray with Catheter in Wrong Position*
*Not the actual radiograph from this case. Catheter tip in the carotid artery; note this was a subclavian approach.
Figure 5. Ultrasound Image of the Right Side of the Neck
C=Carotid artery, RIJ=Right internal jugular vein
Figure 6. Portable Ultrasound Machine for Vascular Access Procedures