The Wet Read
Case Objectives
- Appreciate the limitations of radiology resident emergency coverage.
- Understand the rate of discrepancy between radiology resident preliminary reads and attending radiologists' final readings.
- Understand the alternative approaches to emergency radiology coverage, including teleradiology.
- Realize the limitations on subspecialists' or general radiologists' emergency coverage.
Case & Commentary: Part 1
A 66-year-old man with prostate cancer and known bone metastases presented to the emergency department with a gradual increase in back pain and difficulty ambulating. Initial radiographic evaluation demonstrated stable metastatic bone lesions in the lumbar spine without evidence of cord compression. The patient was admitted for pain control with intravenous morphine and started on patient-controlled analgesia (PCA). Admitting laboratory studies were notable for mild anemia. Renal function, LFTs, and coags were within normal limits. CXR and urinalysis were unremarkable.
On the night of hospital day 2, the patient developed acute shortness of breath and was found to be tachycardic and slightly less responsive. His oxygenation was 78% on room air and 92% when placed on a non-rebreather mask. ECG showed evidence of right heart strain, and a room air blood gas revealed a pH of 7.33, a CO2 of 50, and a paO2 of 55. Given the high suspicion for pulmonary embolism, the resident physician ordered a computerized tomography (CT) angiogram of the lungs. The on-call radiology resident read the study, contacted the ordering physician, and reported that his findings were consistent with a large pulmonary embolism in the right main pulmonary artery. As the patient was mildly hypotensive and had hypoxemic respiratory failure requiring intubation and mechanical ventilation, a decision was made to administer thrombolytic therapy.
The following morning, the patient's condition improved with normalization of blood pressure, improved oxygenation, and increased level of consciousness. While the team was rounding and discussing plans for extubation, the radiology attending called the ICU and reported that the final reading of the CT angiogram showed no evidence of a pulmonary embolism. He explained that what was initially read as a large pulmonary embolus was in fact a large artifact (Box) on the image cut reviewed by the overnight resident.
In teaching hospitals, radiology residents have traditionally provided preliminary interpretations during off-hours for patients in the emergency department and on inpatient wards.(1) In most cases, the only off-hours services provided by attending radiologists were in interventional radiology. For other types of radiologic studies, attending radiologists have generally followed up on preliminary reports (known as “wet-readings”) from night residents the next morning or at certain times on weekends.
Recent studies have shown that the frequency of significant errors by radiology residents is very low. Although minor discrepancies, unlikely to have a significant impact on patient care, have been reported in 3% to 7% of readings, the rate of major discrepancies that may alter patient care ranges from less than 1% to around 2.3% of cases.(2-8) These recent findings are in contrast to a single earlier study that found major and minor discrepancies at a rate of 5% and 11%, respectively.(9) Even with the low discrepancy rates shown in recent studies, several have shown higher discrepancy rates when readings have been performed by the most junior residents.(5,7,10) Interestingly, these overall rates of resident errors are similar to the rate of interobserver differences among attending radiologists. Moreover, the error rates are substantially below those found when attending emergency department physicians' readings are compared with those of attending radiologists.(5)
Nonetheless, concern persists about the unusual instance in which a resident's misread film results in a patient being sent home without appropriate treatment or in a patient receiving improper surgery or other therapies. Many faculty in academic radiology departments have debated appropriate off-hours coverage for years. These debates must weigh the fact that residents' off-hours experience is an important part of their professional development, building their confidence and judgment in a semi-independent environment.(6)
Case & Commentary: Part 2
In light of the new reading, the team decided the clinical decompensation was likely due to aspiration and mucous plugging secondary to oversedation from narcotics. The right heart strain noted on ECG was determined to be an old finding from mild unexplained pulmonary hypertension. The patient did not have bleeding complications from the thrombolytic therapy. He was extubated and ultimately discharged to a skilled nursing facility for rehabilitation.
Fortunately, no harm came to the patient in this case. But it might have. How could this error have been prevented? Attending radiology faculty could certainly provide off-hours coverage, but few would want to work through the night on a regular basis. Large radiology departments tend to have very busy night schedules for CT and plain radiographic images. Typically, academic departments are filled with radiologic subspecialists (eg, chest, abdomen, or MRI) who often have limited their practices to selected areas and do not feel comfortable covering cases outside their area. For such departments to provide off-hours coverage with faculty would be difficult indeed, requiring multiple subspecialists to be on every night.
Another approach has been the use of general radiologists reading the films remotely through teleradiology.(11) These radiologists can cover a number of hospitals at the same time. Private practice radiologists use these services (which may involve domestic or international teleradiology) much more frequently than academic departments, where residents perform overnight coverage. As these general radiologists lack the subspecialty training found in academic centers, the quality of service may be less.(12) And if a general radiologist only provides the preliminary report and the subspecialist academic faculty reads the film again the next morning, the costs for the services may become quite high, since only one interpretation will be reimbursed.
When radiology trainees provide preliminary reports, back-up support by attending faculty for difficult cases must be readily available. Often, faculty provide coverage from home through web-based access to the Picture Archive and Communications System (PACS).(1) An attending with high-speed internet access can review a single case or a few cases from home overnight. It would, however, be very difficult to provide this level of review for all cases because home access may be slower and offer fewer features than the typical PACS workstation in the hospital.
Residents on call are often reluctant to call the attending faculty, fearing that such calls would signal that they are not capable of handling the situation themselves. To help decrease this underutilization, many departments have established rules for when a resident needs to seek assistance. Ideally, no patient would undergo surgery or other invasive procedure based on radiographic findings without an attending radiologist's review. A safeguard such as this (if extended to the use of thrombolytic therapy) may have prevented the error in this case. In addition to these criteria, when a referring physician in the emergency department or elsewhere in the hospital wishes to have an attending radiologist's review for whatever reason, they should be able to trigger that home review.
Timely next-day review of off-hours cases and immediate communication of discrepancies in interpretation are critical. These cases must be reviewed early enough in the day to provide the referring physicians comfort that further actions (such as surgery) will be based on the most up-to-date and accurate information from the imaging studies. Residents' preliminary interpretations should be conveyed in writing to the requesting physician. Whenever there is a discrepancy after attending review, these changes need to be immediately communicated with the referring physician with a clear indication of the change. If the referring physician has taken action on the patient based on an erroneous preliminary report, that physician needs to be able to refer to the original reading if there is any question about the care.
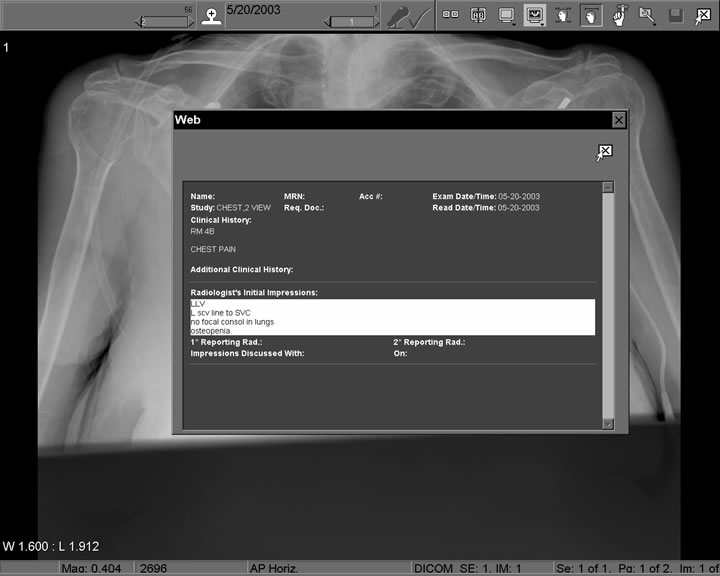
To provide the safety net for these resident preliminary readings while protecting the residents' training experience, the UCSF department of radiology developed a “wet-read” computer system (Figures 1, 2, and 3).(13) This system provides the resident with a convenient report generation system for preliminary findings, which are immediately communicated to referring physicians either on their PACS workstation or via pagers or hand-held devices. The next morning, the attending radiologist indicates agreement with the resident report or indicates a change, the magnitude of the change, and whether it might alter care for the patient.
This automated system also allows for emergency department physicians to record their image findings, especially if they reviewed the images before the radiology resident or attending. If the resident finds an abnormality missed by the emergency department physician, he or she calls right away to alert them. All of these preliminary reports are stored in the computer system permanently, although the dictated report and then the finalized report replace them as the most-up-to-date information displayed when the patient's medical record is accessed. This system also automatically records discrepancies and provides reports indicating the frequency and significance of errors for all physicians involved. Our system has found error rates similar to others that have been published: 0.47% major, 4.00% minor, 1.52% questionable, and 94.01% no errors.
The frequency of significant errors by radiology residents is very low when compared with attending reviews the next day. Nevertheless, errors do occur and their implications can be severe if they result in inappropriate triage or therapy. Because having full-time coverage by academic radiologists does not currently seem feasible and teleradiology provided by general radiologists may be inferior to that provided by subspecialty radiologists, perhaps “higher-risk” cases could be identified and lead to automatic attending back-up reads. For example, higher-risk cases might include those read by more junior reviewers, or those whose interpretations could prompt procedures or life-threatening therapies. In addition, formal policies could be created to trigger involvement of the attending and efforts could be made to change the culture to increase resident willingness to involve the attending. Ideally, all institutions would have computer systems that would ease provision of off-hours coverage from home and facilitate timely communication with referring physicians.
Take-Home Points
- Radiology residents provide excellent emergency coverage off-hours, but some significant errors do occur.
- Junior residents make more mistakes than more senior residents, fellows, or faculty.
- Without subspecialist review the next day, general radiologists who cover off-hours, often via teleradiology, appear to make more errors than residents.
- Attending radiologists need to provide back-up for the residents, and can do so by accessing the images remotely via PACS.
- Computer systems can record the frequency and significance of the discrepancies between the residents' and attendings' readings and help improve communication of such discrepancies with referring physicians.
Ronald L. Arenson, MD Chairman and Alexander R. Margulis Distinguished Professor Department of Radiology University of California, San Francisco
Faculty Disclosure: Dr. Arenson has declared that neither he, nor any immediate member of his family, has a financial arrangement or other relationship with the manufacturers of any commercial products discussed in this continuing medical education activity. In addition, his commentary does not include information regarding investigational or off-label use of pharmaceutical products or medical devices.
References
1. Hunter TB, Krupinski EA, Hunt KR, Erly WK. Emergency department coverage by academic departments of radiology. Acad Radiol. 2000;7:165-170. [ go to PubMed ]
2. Wechsler RJ, Spettell CM, Kurtz AB, et al. Effects of training and experience in interpretation of emergency body CT scans. Radiology. 1996;199:717-720. [ go to PubMed ]
3. Yoon LS, Haims AH, Brink JA, Rabinovici R, Forman HP. Evaluation of an emergency radiology quality assurance program at a level I trauma center: abdominal and pelvic CT studies. Radiology. 2002;224:42-46. [ go to PubMed ]
4. Roszler MH, McCarroll KA. Rashid T, Donovan KR, King GA. Resident interpretation of emergency computed tomographic scans. Invest Radiol. 1991;26:374-376. [ go to PubMed ]
5. Wyoski MG, Nassar CJ, Koenigsberg RA, Novelline RA, Faro SH, Faerber EN. Head trauma: CT scan interpretation by radiology residents versus staff radiologists. Radiology. 1998;208:125-128. [ go to PubMed ]
6. Carney E, Kempf J, DeCarvalho V, Yudd A, Nosher J. Preliminary interpretations of after-hours CT and sonography by radiology residents versus final interpretations by body imaging radiologists at a level 1 trauma center. AJR Am J Roentgenol. 2003;181:367-373. [ go to PubMed ]
7. Erly WK, Berger WG, Krupinski E, Seeger JF, Guisto JA. Radiology resident evaluation of head CT scan orders in the emergency department. AJNR Am J Neuroradiol. 2002;23:103-107. [ go to PubMed ]
8. Lal NR, Murray UM, Eldevik OP, Desmond JS. Clinical consequences of misinterpretations of neuroradiologic CT scans by on-call radiology residents. AJNR Am J Neuroradiol. 2000;21:124-129. [ go to PubMed ]
9. Velmahos GC, Fili C, Vassiliu P, Nicolaou N, Radin R, Wilcox A. Around-the-clock attending radiology coverage is essential to avoid mistakes in the care of trauma patients. Am Surg. 2001;67:1175-1177. [ go to PubMed ]
10. van Rossum AB, van Erkel AR, van Persijn van Meerten EL, Ton ER, Rebergen SA, Pattynama PM. Accuracy of helical CT for acute pulmonary embolism: ROC analysis of observer performance related to clinical experience. Eur Radiol. 1998;8:1160-1164. [ go to PubMed ]
11. Wachter RM. International teleradiology. N Engl J Med. 2006;354:662-663. [ go to PubMed ]
12. Kangarloo H, Valdez JA, Yao L, et al. Improving the quality of care through routine teleradiology consultation. Acad Radiol. 2000;7:149-155. [ go to PubMed ]
13. Tellis WM, Andriole KP. Integrating multiple clinical information systems using the Java message service framework to enable the delivery of urgent exam results at the point of care. J Digit Imaging. 2005;18:316-325. [ go to PubMed ]
Figures
Figure 1. Radiologist's Form for Entering Wet Read
Click on thumbnail to view full-size image
Figure 2. View from PACS Display
Figure 3. Form for Entering Attending's Q/A Review
Box
|
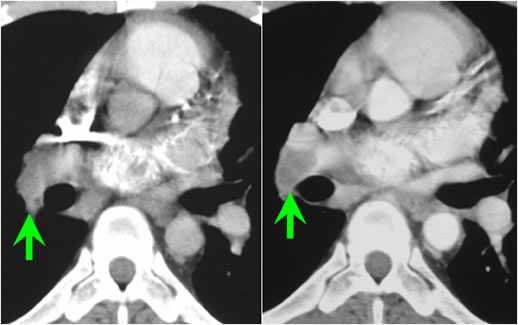
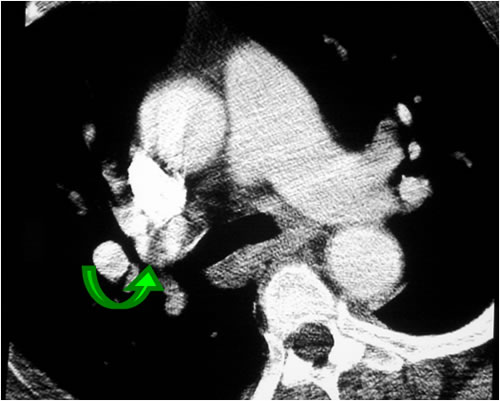
Diagnostic Pitfalls of CT Angiography for Evaluating Pulmonary Embolism Sidebar by Michael B. Gotway, MD Helical CT is being increasingly utilized for the evaluation of suspected pulmonary embolism (PE). Proper scan interpretation depends on the awareness of several diagnostic entities that may simulate PE, including normal bronchovascular structures such as pulmonary veins, bronchi, and lymph nodes. In addition, technical issues can create pitfalls that lead to misdiagnoses; these include improper bolus timing (Figure A) and streak artifacts (Figure B), as well as patient motion artifacts, pulmonary arterial catheters, and vascular shunts (Table). When radiologists read scans looking for signs of PE, they are searching for filling defects within a blood vessel (ie, the contrast either stops abruptly or is seen around a central defect). In this case, it was determined that an artifact was mistaken for PE in the right main pulmonary artery. There are only a few artifacts that could mimic PE in the right main pulmonary artery, since this vessel is very central. Although uncommon, flow artifacts may simulate PE. Because most vessels have laminar blood flow (with flow faster in the center of the vessel than at the periphery), a late-timed contrast bolus may create the appearance of contrast at the periphery of the vessel and unopacified blood in the center, simulating PE. Of the possible causes mentioned above, the only other causes that might lead to a mistaken call of PE in a central vessel are streak artifacts, cardiac motion, the tip of a pulmonary artery catheter, and lymph nodes. This patient was ultimately diagnosed with bronchial mucoid impaction. Remember that the radiologist searching for possible PE is looking for a round structure with something dark in the middle. Impacted bronchi may have this appearance, since the bronchial wall is usually slightly denser than the low-attenuation mucus within the lumen, especially if the bronchial wall is calcified. The distinction between a plugged bronchus and a PE can be difficult, because the pulmonary arteries and bronchi run together. Because of this co-location, it is important to pay close attention to the anatomy. Because the right pulmonary artery is such a large central structure, mucoid impaction is not likely to be misinterpreted as PE in this vessel. Rather, this mistake usually occurs at the lobar, segmental, and subsegmental vessels. Michael B. Gotway, MD Scottsdale Medical Imaging Clinical Associate Professor, Diagnostic Radiology and Pulmonary/Critical Care Medicine Department of Radiology University of California, San Francisco Faculty Disclosure: Dr. Gotway has declared that neither he, nor any immediate member of his family, has a financial arrangement or other relationship with the manufacturers of any commercial products discussed in this continuing medical education activity. In addition, his commentary does not include information regarding investigational or off-label use of pharmaceutical products or medical devices.
Figure A. Example of CT Showing Improper Bolus Timing Image on left shows poor enhancement of pulmonary vasculature due to early contrast bolus. Note that contrast is primarily within right ventricular outflow tract and has not yet reached aorta. Poor enhancement of right interlobar pulmonary artery (arrow) causes difficulty in PE diagnosis. Image on right obtained with correct contrast bolus timing shows excellent pulmonary artery enhancement, allowing diagnosis of PE (arrow).
Figure B. Example of CT Showing Streak Artifact Axial CT image shows decreased attenuation affecting right upper lobe pulmonary artery (arrow), potentially simulating PE. Decreased attenuation is caused by streak artifact emanating from dense contrast column in superior vena cava.
|