Telehealth and Patient Safety.
O'Malley G, Shaikh U, Marcin JP. Telehealth and Patient Safety.. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2022.
O'Malley G, Shaikh U, Marcin JP. Telehealth and Patient Safety.. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2022.
Background
In recent years, telehealth, or the delivery of healthcare over a distance using telecommunications technologies, has had a dramatic impact on the modalities and models of healthcare delivery used by healthcare practices and health systems throughout the country.1 Its exponential expansion, spurred by the COVID-19 pandemic, has been further facilitated by the removal of restrictive policies and regulations by both federal and state governments. The relaxation of originating site restrictions, the opportunity for parity in payment, and a broadening of which types of clinicians can use telehealth for services all have added to the increased adoption of telehealth.
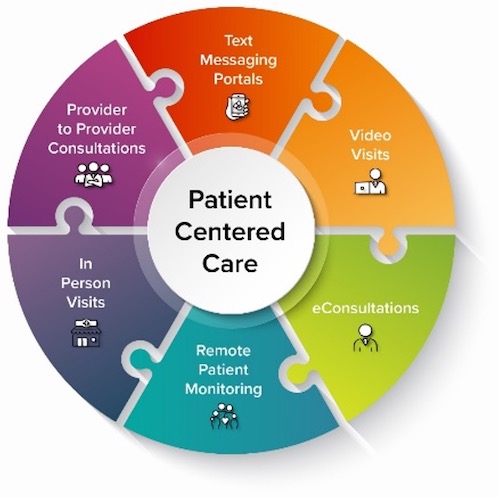
With expanded use, there has also been an increase in how telehealth technologies are used in clinical practice, providing a portfolio of options for patients and providers that include provider-to-patient visits, provider-to-provider consultations, eConsultations, text and messaging portals, remote patient monitoring technologies, and hybrid models that leverage both synchronous and asynchronous technologies (Figure).2 The rapid expansion of telehealth and the variation in implementation of new models of care into medical practice has resulted in emerging concerns regarding patient safety.3
These concerns are exacerbated by the fact that clinical practices and health systems were obliged to rapidly implement telehealth into existing operations with the onset of the COVID-19 pandemic, which reduced the time and opportunity for healthcare operations or providers to hardwire processes and measures to ensure patient safety and equity. While many of the safety concerns surrounding telehealth are similar to concerns raised with in-person care, specific considerations related to patient safety have emerged given the unique modalities of care in telehealth.
Figure. Modalities of digital and telehealth delivery
Patient Safety Concerns
Diagnostic errors
Several features of telehealth visits can contribute to diagnostic errors: (1) inadequate medical history-taking due to poor communication, (2) very limited physical examinations, omitting key modalities such as auscultation and private or inaccessible areas of the body, (3) reliance on patients and their families to measure vital signs or describe physical findings.
Use of telehealth services with providers who are not a part of the patients’ routine care team has been associated with the requirement for higher in-person follow-up care raising patient safety concerns.4 However, it is believed that these risks can be mitigated when telehealth is provided by clinicians within the patient’s existing medical home where there is access to the patient’s medical records and the physician can arrange for testing, follow-up, and place specialist referrals.
In some circumstances, a clinician’s care over telehealth might result in more accurate and honest information gathering. Compared to patients interacting with physicians in-person, patients are more likely to accurately disclose information over telehealth. People who are directly interacting with computers report lower fear of disclosure and display emotions more intensely than if interacting with humans.5 While this is a potential benefit of telehealth in terms of patient safety, some telehealth models of care have also been shown to be associated with lapses in communication and patient engagement. For example, routine screening for mental and behavioral health issues with questionnaires administered prior to encounters for depression, anxiety, and substance abuse may be completed less frequently than with in-person visits.
Medication safety
Sub-optimal communication could affect the quality of medication reconciliation and lead to adverse drug events, especially if telehealth models do not intentionally integrate multidisciplinary team members such as pharmacists, to ensure detailed medication reconciliation. Variation in patient literacy, health literacy, and English proficiency, as well as technology access and skills affect medication reconciliation and the delivery of counseling on medication use. Patient safety could be compromised if telehealth encounters do not integrate easy access to tools such as after visit summaries to communicate medication regimens.
When telehealth has been used for on-demand clinical calls using systems and providers that are not a part of the patient’s medical home, some research indicates that quality may be lower than in-person care.6 However, when providers use telehealth to engage with their own patients, patient satisfaction and clinical outcomes are improved. Research has shown that patient satisfaction with telehealth encounters is similar to, and in some cases higher than, in-person encounters when the telehealth providers are from their existing in-person practice.7 Better patient experience of care is associated with greater compliance with clinician recommendations, adherence to recommended therapies, and fewer missed follow-up visits.
Escalation of care
Remote patient monitoring with peripheral medical devices such as pulse oximetry, blood pressure cuffs, and scales, and remote monitoring of existing medical devices such as glucose monitors and insulin pumps can increase patient safety by proactively monitoring for alterations in medical conditions. While research results have been mixed, monitoring of patients with chronic medical conditions such as congestive heart failure, hypertension, diabetes, and chronic obstructive pulmonary disease can improve patient safety by reducing the frequency of medical exacerbations. In patients with acute conditions, such as COVID-19, at-home daily assessments of pulse oximetry and home monitoring were effective in identifying patients who required an emergency department visit for evaluation and hospitalization as well as lower mortality.8,9
Health equity considerations
Prior to the COVID-19 pandemic, telehealth was primarily used to increase healthcare access for rural communities and populations with complex, chronic medical conditions.10 Telehealth improved access to care and patient safety by increasing adherence to the evidence-based visit guidelines and reducing delays in care and missed appointments.11,12 However, the quick transition to telehealth during the COVID-19 pandemic resulted in telehealth being forced into existing health care delivery and operational workflows that can potentially exacerbate disparities in access to telehealth. For example, research has found that older adults, racial and ethnic minorities, and less resourced individuals are less likely to receive telehealth care compared to in-person and telephone care.13 Telehealth workflows and models that consider social determinants of health and monitor patient measures for populations that are vulnerable to unequal adoption could help reduce patient safety hazards.14
Telehealth Implementation Strategies to Enhance Patient Safety
Strategies to enhance patient safety require attention to effective implementation, education, safety protocols, and strategies around continuous quality improvement. These strategies offered by the authors include:
- Clinician education on the above patient safety considerations and best practices and evidence-based strategies for conducting telehealth encounters, including effective communication skills,
- Maintaining coordinated care within the medical home and limiting care fragmentation whenever possible,
- Integrating protocols in telehealth operations to determine clinical circumstances where telehealth has the potential to negatively impact patient safety, ongoing review of protocols, safety reports, patient feedback, and multi-disciplinary team monitoring,
- Integrating tools that are easily accessible by patients and their caregivers to communicate medication regimens and care plans, and
- Ongoing research to better define what types of care are safely administered using telehealth and assessing the impact of individual patient factors, social determinants of health, and the fidelity of the telehealth care model.
Grace O'Malley, PhD
Senior Lecturer
RCSI University of Medicine and Health Sciences (Dublin, Ireland)
graceomalley@rcsi.ie
Ulfat Shaikh, MD, MPH, MS
Associate Editor, AHRQ’s Patient Safety Network (PSNet)
Professor, Department of Pediatrics
Medical Director for Healthcare Quality
UC Davis Health
ushaikh@ucdavis.edu
James Marcin, MD, MPH
Director, UC Davis Center for Health and Technology
UC Davis Health
jpmarcin@ucdavis.edu
References
- Friedman AB, Gervasi S, Song H, et al. Telemedicine catches on: changes in the utilization of telemedicine services during the COVID-19 pandemic. Am J Manag Care. 2022;28(1):e1-e6. [Free full text]
- De Simone S, Franco M, Servillo G, et al. Implementations and strategies of telehealth during COVID-19 outbreak: a systematic review. BMC Health Serv Res. 2022;22(1):833. [Free full text]
- Baker DW. Improving the quality and safety of telehealth: a call for papers on telehealth. Jt Comm J Qual Patient Saf. 2021;47(7):401-402. [Free full text]
- Hatef E, Lans D, Bandeian S, et al. Outcomes of in-person and telehealth ambulatory encounters during COVID-19 within a large commercially insured cohort. JAMA Netw Open. 2022;5(4):e228954. [Free full text]
- Lucas GM, Gratch J, King A, et al. It's only a computer: Virtual humans increase willingness to disclose. Comput Hum Behav. 2014;37:94-100. [Free full text]
- Uscher-Pines L, Mulcahy A, Cowling D, et al. Access and quality of care in direct-to-consumer telemedicine. Telemed J E Health. 2016;22(4):282-287. [Free full text]
- Hays RD, Skootsky SA. Patient experience with in-person and telehealth visits before and during the COVID-19 pandemic at a large integrated health system in the United States. J Gen Intern Med. 2022;37(4):847-852. [Free full text]
- Aalam AA, Hood C, Donelan C, et al. Remote patient monitoring for ED discharges in the COVID-19 pandemic. Emerg Med J. 2021;38(3):229-31. [Free full text]
- Padula WV, Miano MA, Kelley MA, et al. A cost-utility analysis of remote pulse-oximetry monitoring of patients with COVID-19. Value Health. 2022;25(6):890-6. [Free full text]
- Kaufman T, Geraghty EM, Dullet N, et al. Geospatial information system analysis of healthcare need and telemedicine delivery in California. Telemed J E Health. 2017;23(5):430-4. [Available at]
- Dayal P, Chang CH, Benko WS, et al. Appointment completion in pediatric neurology telemedicine clinics serving underserved patients. Neurol Clin Pract. 2019;9(4):314-21. [Free full text]
- Dayal P, Chang CH, Benko WS, et al. Hospital utilization among rural children served by pediatric neurology telemedicine clinics. JAMA Netw Open. 2019;2(8):e199364. [Free full text]
- Eberly LA, Kallan MJ, Julien HM, et al. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 Pandemic. JAMA Netw Open. 2020;3(12):e2031640. [Free full text]
- Bailey JE, Gurgol C, Pan E, et al. Early patient-centered outcomes research experience with the use of telehealth to address disparities: scoping review. J Med Internet Res. 2021;23(12):e28503. [Free full text]