Delayed Evaluation of Abdominal Pain in an Elderly Patient.
Klimkiv L, Utter GH, Barnes DK. Delayed Evaluation of Abdominal Pain in an Elderly Patient.. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2023.
Klimkiv L, Utter GH, Barnes DK. Delayed Evaluation of Abdominal Pain in an Elderly Patient.. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2023.
The Case
An 85-year-old woman presented to the Emergency Department (ED) at 1800H complaining of abdominal pain that had started that morning. She was alert and conversant. The ED was crowded, so she was queued into a long line of patients waiting to be triaged. She was seen by a triage nurse at 2000H and again reported generalized abdominal pain, which she rated as 7 on a 0-10 scale. She also reported decreased appetite; her last meal was a light breakfast around 0600H. She denied vomiting, diarrhea, or constipation. Her vital signs included blood pressure 110/73 mmHg, heart rate 104 beats per minute, respirations 16 per minute, oxygen saturation 97% on room air, and oral temperature 96.5˚F. On a brief physical examination, her skin was pale, warm, and dry, and abdominal guarding was absent. She was assigned an Emergency Severity Index (ESI) score of 3 and was triaged to the waiting room until a treatment bed became available. Although the patient repeatedly asked staff when she would be roomed, she continued to be cooperative. By 2100H, she was placed in a hallway treatment space and triage orders were initiated by protocol. An intravenous infusion of normal saline was started at 500 mL/hour. At around 2130H, an abdominopelvic computed tomography (CT) scan without contrast was completed and she returned to the hallway.
At 2235H, the ED physician was contacted by the hospital’s on-call radiologist who reported seeing extensive bowel necrosis on the CT scan. The patient was roomed at 2300H. The ED physician informed the assigned nurse that the patient was in critical condition. She was connected to a cardiac monitor, which showed sinus tachycardia at 110 and blood pressure 105/69. Her serum lactate level returned at 12 mmol/L (reference range 0.3 - 2.2 mmol/L). The ED physician ordered isotonic fluids and broad-spectrum intravenous antibiotics, which were administered quickly. Low dose morphine and fentanyl were given to relieve pain. A surgical consultant deemed the patient to be inoperable and non-recoverable due to extensive bowel necrosis. The patient’s family was notified, and she was admitted for comfort care. The patient remained alert and cooperative until 2350H when her blood pressure fell to 90/58. She started to vomit blood a few moments later, was transferred to an inpatient room within 30 minutes, and died 30 minutes later.
The Commentary
by Liliya Klimkiv, MD, Garth Utter, MD, MSc, and David K. Barnes, MD
This case describes an older adult patient with generalized abdominal pain who was eventually diagnosed with inoperable bowel necrosis. Although she appeared well and had stable vital signs, triage was delayed due to ED crowding, which is usually a result of hospital crowding. She was under-triaged and waited three hours before any diagnostic studies or interventions commenced. Once she was placed on a hallway gurney—which should not be considered an appropriate or adequate treatment area—laboratory and imaging studies proceeded hastily. Catastrophic bowel necrosis was eventually identified, yet she was not moved to a standard ED treatment bed for another 25 minutes. Despite aggressive resuscitation, the surgeon determined that operative intervention was futile, and the patient died a short time later.
It is unclear whether the patient might have survived had the diagnosis been made more expeditiously. Like many intra-abdominal catastrophes, such as ruptured abdominal aortic aneurysm, bowel necrosis is associated with high mortality under the best of circumstances.1 Nevertheless, every patient deserves to be provided with the best opportunity to survive an illness or injury. This requires timely assessment and diagnosis.
Approach to Improving Patient Safety
The impulse to blame crowding for the poor outcome is understandable and partly accurate. When many patients arrive at the ED simultaneously, even robust triage systems and efficient processes of care become overwhelmed. However, other factors undoubtedly contributed to the negative outcome in this case.
First, not all patients present with the same level of risk, and triaging patients as if they are homogenous risks over- and under-triage. The ESI triage process is insensitive to the nuances in patient presentations. While ESI addresses age in pediatric patients, it makes no distinction between older and younger adults. Triage tools should be improved to better identify high-risk presentations, given anatomic and physiologic differences between older and younger adults that may mask illness severity in the former. It is imperative that physicians and nurses recognize these differences across age groups and adapt the way they assess, evaluate, and manage older adult patients.
Once a life-threatening process is identified, appropriate patient care should proceed rapidly. Patients should be moved to a location that permits all necessary interventions to be provided commensurate with the degree of illness or injury. A hallway gurney is an unmonitored “treatment space” that lacks both necessary resources (e.g., cardiac monitor) and privacy, each essential for high-quality patient care.
Furthermore, as EDs face historic volumes of patients and high levels of boarding and crowding, ED staff must improve workflows to maximize patient safety. Many patients who come to the ED do not need extensive workups and use few resources. Split flow models of care assure patients receive the right resources in the right location at the right time. Rather than leaving patients—some with serious pathology despite reassuring presentations—to linger in the waiting room after triage, EDs can create parallel processes of care by shifting diagnostic studies, and even some therapeutic interventions, to an earlier point in the patient’s ED journey. The following sections describe these processes in more detail.
Abdominal Pain in Elderly Patients
Abdominal pain in geriatric patients is a challenging chief complaint. Compared to younger patients, geriatric patients are less likely to present with typical symptoms. Delayed presentation is common due to age-related changes in peripheral nerve function that dull perception and impair pain localization. Physical examination is often limited due to abdominal muscle atrophy, which can mask rebound and guarding. Clinicians who rely on classic findings to detect acute surgical emergencies in the older adult may be misled.2 Medical comorbidities and polypharmacy may also complicate the presentation of abdominal pain in older adults. Many common medications, such as beta blockers, blunt the response to inflammation and infection.3 Not surprisingly, morbidity is three-fold higher for patients over 70 years who present to the ED with acute abdominal pain, compared with younger patients.4 Nearly half of geriatric patients presenting with acute abdominal pain require admission, and roughly one third require surgical intervention.2,5 Elderly patients presenting with abdominal pain should therefore be considered higher risk and assigned higher triage priority. Emergency physicians should have a low threshold to obtain abdominal imaging in older adult patients, even in those with a benign physical examination and reassuring vital signs.6
Triage
ED staff are charged with allocating appropriate resources to patients with emergency medical conditions. Triage serves to sort and prioritize patients by severity of illness when resources are not available to treat them immediately. In the United States, 96% of EDs utilize the Emergency Severity Index (ESI), a triage tool that sorts patients into five groups from most urgent (ESI-1) to least urgent (ESI-5) based on vital signs, visual assessment, and anticipated resource needs.7 Although ESI is able to differentiate high and low acuity patients, it has flaws. Triage quality improvement that includes regular feedback can ensure appropriate application of the algorithm and avoid mistriage. A previous PSNet Commentary addressing delayed diagnosis of a ruptured aortic aneurysm discussed the triage process in detail. Based on this patient’s chief complaint (abdominal pain in an older adult patient), expected resource utilization (i.e., laboratory tests, imaging, and consultation/admission), and tachycardia (104) at triage, she should have been assigned ESI-2 instead of ESI-3. Doing so could have expedited her transfer from the waiting room to a treatment bed and may have led to an earlier diagnosis.
Early in their development, triage assessments were limited in scope and intended to be completed within 10-15 minutes of the patient’s arrival.8 However, ED volumes have reached levels that strain the ability of staff to triage patients quickly. Moreover, modern triage requires significantly more time to complete. Triage requirements imposed by regulatory entities, including the Centers for Medicare & Medicaid Services (CMS) and The Joint Commission (TJC), demand screening for suicide risk, travel to high-risk countries, infectious disease symptoms, intimate partner violence, and sex trafficking. A brief nursing assessment, based on a focused history and exam, is still required to be charted for every patient. Some presenting chief complaints prompt point of care testing, such as electrocardiograms for patients with chest pain and glucose measurement for patients with diabetes. Patients who require interpreting services take longer to triage. All these factors add significant time beyond evaluation of the chief complaint and frequently lead to delayed triage for subsequent patients. Adequate ED staffing should be available to triage patients in a timely manner; flexing staff when ED volume surges may become necessary.
With extended ED waiting times, patients should be reassessed frequently, and their ESI category should be updated if their status changes. This is especially important for older adult patients because under-triage is common in this patient population.4,9 Unfortunately, it took two hours to triage the patient because of a long queue, far exceeding the optimal arrival-to-triage time. The reason for the triage delay is unclear, but triage can easily back up when the ED is busy, given triage activities that exceed cursory requirements. The resulting delays compromise safety for patients with time-sensitive emergencies.
Crowding and Boarding
As previous PSNet Cases and Commentaries have described, ED and hospital crowding are major public health risks in the US and worldwide. Although the primary mission of the ED is to treat life-threatening emergencies, the modern ED serves a much broader function. When access to primary and preventive care is limited, EDs serve as a safety net, providing on-demand care, after hours care, weekend care, and a “one-stop” location for unscheduled care, and a resource for circumstances that are not true emergencies but shouldn't require weeks- or months-long wait times for outpatient evaluation. With the closure of many state-funded mental health hospitals in the 1980s, EDs are on the front lines of the nation’s mental health crisis.
ED crowding is a phenomenon created when there is no physical space or resources to meet the timely needs of the next patient who needs emergent care. Conceptually, ED crowding can be attributed to input factors, throughput factors, and output factors. One output factor, ED boarding, is recognized as having the greatest impact on ED crowding and occurs when the hospital is at full inpatient capacity and admitted patients are held in the ED.10Boarding decreases the number of physical spaces in the ED to see new patients, and both crowding and boarding may lead to delayed diagnosis, which may in turn increase the risk of death. ED boarding also increases hospital length of stay, patients leaving the ED without being seen, medical errors, and ambulance diversion.11-15 Although the state of crowding and boarding when the patient arrived is unknown, the fact that she waited two hours to be triaged and was then placed in a hallway gurney suggests that both factors were operative. Had she been placed in a treatment room and evaluated earlier, her condition would have been diagnosed and managed more expeditiously.
Improved ED Throughput
Inputs to the ED are difficult to mitigate. Despite efforts to reduce ED utilization, patient access to emergency care is protected by federal statute. Improving throughput, however, is within the ED’s sphere of influence and can decrease ED crowding. Rapid visual assessment, split flow models of care, and rapid medical evaluations are three processes that can increase ED throughput so that more patients can be treated more quickly.
Rapid Visual Assessment
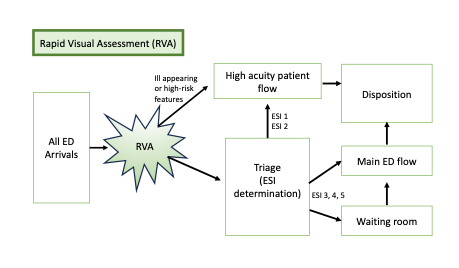
Our hospital added a rapid visual assessment (RVA) team to the triage process (Figure 1). RVA is a “pre-triage” step, a physical space located at the entrance to the ED where patients are quickly assessed by an experienced triage nurse using the patient’s chief complaint, appearance, and nursing gestalt. Patients with high-risk complaints (e.g., stroke symptoms) are prioritized for triage. Those whose visual assessment suggests a life-threatening physiologic or anatomic derangement (e.g., patients who are unresponsive, cyanotic, seizing) bypass triage altogether and are roomed immediately. This process improves patient safety by “pre-sorting” patients prior to formal triage and rapidly identifying those patients who need immediate care. When the triage queue is long, RVA provides a mechanism to prioritize otherwise stable patients awaiting triage.
Figure 1. Rapid visual assessment process
Split Flow Model (aka Fast Track)
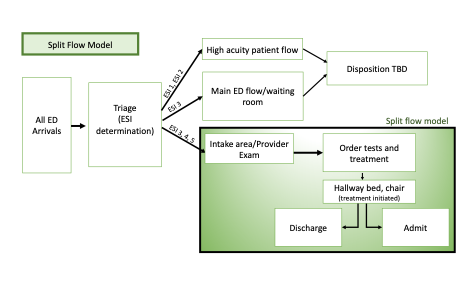
ED patients are heterogenous; identifying low acuity patients with minor complaints and directing them to an area focused on rapid diagnosis and treatment frees resources for sicker, high acuity patients. The split flow model of care—often referred to as Fast Track—is a common and effective mechanism to rapidly assess, treat, and usually discharge stable patients who require limited resources (Figure 2). Criteria vary by institution, but patients are most often identified at triage using specific clinical criteria and ESI categories 4 and 5; some ESI 3 patients may also qualify. Split flow models have demonstrated decreased length of stay, improved throughput, reduced rate of leaving before treatment is completed (LBTC), reduced ED crowding (without increasing ED readmissions or mortality), and increased patient satisfaction.16-18 To avoid poor patient outcomes, ED staff should be prepared to up-triage patients whose condition is later identified to require more resources and a higher level of care.
Split flow models are safe for older patients because of the detrimental effects of prolonged ED length of stay in the geriatric population, including increased risk of delirium, hospital admission, and in-hospital mortality.19 Although the current patient would not have met criteria for Fast Track treatment, the improved efficiency to the overall system of care can increase throughput and thus decrease ED crowding.
Figure 2. Example of a split flow model of care
Rapid Medical Evaluation
ED workflows traditionally rely on sequential, linear processes of care. For example, a patient presents to triage and, if stable, goes to the waiting room until a treatment bed is available. Once there, they wait to see a licensed provider who then orders diagnostic testing. Once the results become available, treatment commences and eventually the patient is dispositioned. This process is inefficient and thus unsafe in a busy ED.
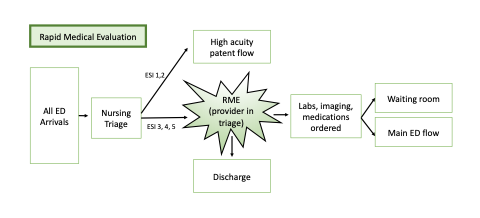
The rapid medical evaluation (RME) process (Figure 3), which we implemented to address higher ED volumes and boarding-related crowding, moves diagnostic testing and some treatment interventions to the point of triage. During triage, a licensed provider quickly evaluates the patient and initiates diagnostic testing and treatment. Rather than waiting (sometimes many hours) for testing to commence in a room, patients are immediately queued for radiology studies and laboratory testing. Therapeutic interventions, such as intravenous fluids, analgesics, and antibiotics are also initiated. Patients may shuttle to and from the waiting room for testing, or they may be placed in a monitored staging area with chairs and exam tables. Such parallel processes of care can significantly shorten the interval from arrival to disposition, especially when diagnostic studies are completed before rooming.20
RME, alternately referred to as a Provider-in-Triage (PIT) model, is not without criticism. Because a PIT provider’s time with a patient is brief compared to a full evaluation in a treatment space, both over-testing and over-treatment may result.21 Therefore, EDs that choose these “front-end” models of care should be monitored for trends in resource utilization to ensure that quality and value are not compromised in the interest of efficiency. Our RME process includes alerts in the electronic health record that notify a dedicated flow nurse when all diagnostic studies have resulted, allowing patients to be re-triaged based on the results. Patients with abnormal results are prioritized for ED beds, while patients with normal studies may be appropriate for Fast Track or expedited discharge by a provider from the triage area.
Figure 3. The rapid medical evaluation
ED crowding can also be mitigated by using Advanced Practice Providers, increasing ED staffing during peak ED hours, expanding ED bed capacity, improving turn-around times for radiology and laboratory studies, and using care coordinators to assist with discharge planning. Many of these high-impact solutions are recommended by the American College of Emergency Physicians (ACEP) Emergency Medicine Practice Committee.22
Verifying the Diagnosis and Prognosis
The case description concludes with the patient rapidly deteriorating after radiographic detection of extensive infarction of the intestines, with a quick shift to providing comfort care. Although occasional patients become so physiologically unstable that general anesthesia cannot be administered without risking sudden death, surgeons must err on the side of being proactive if operative treatment of the underlying condition (e.g., surgical control of bleeding or the source of sepsis) would offer the only real possibility of interrupting the patient’s physiologic deterioration. Diagnosis of acute mesenteric ischemia by computed tomography can be challenging and requires intravenous contrast.23 Specifically, this imaging modality cannot enable precise estimates of the severity, reversibility, and anatomic extent of ischemia— information necessary to ascertain the patient’s prognosis.
Surprisingly, given inherently limited information and a short period of evaluation, the patient’s surgeon deemed the patient inoperable. It is unclear if the patient’s care preferences, comorbidities, or perhaps understated physiologic instability may have contributed to the surgeon’s decision-making, but surgeons at our center typically offer exploratory laparotomy or laparoscopy to at least verify a diagnosis of acute mesenteric ischemia and determine its prognosis. If the surgeon were to encounter extensive necrosis or irreversible ischemia of the intestines, they would conclude the procedure (without removal of any of the affected intestine) and focus subsequent care on maximizing the patient’s comfort. However, if at least 150 cm of small intestine remains viable (100 cm if the ileocecal valve remains), the patient could undergo aggressive resection of the affected intestine and potentially survive without “short bowel syndrome.” (And recent series suggest that the necessary threshold of residual small intestine may be even shorter.24,25) Acute mesenteric ischemia is a major challenge for any 85-year-old to overcome, but prematurely foreclosing surgical management will certainly result in the patient’s death. In high-stakes, time-pressured circumstances, surgeons must navigate these challenges to match care to the patient’s preferences as best they can.
Take-Home Points
- Even if the physical exam is reassuring, older adult patients with abdominal pain have a high incidence of surgical pathology. These patients should be considered “high risk,” and clinicians should have a low threshold for abdominal imaging.
- Triage is the process of prioritizing and sorting patients when resources are limited. EDs should flex staffing to support triage when triage systems get overwhelmed from many patients arriving simultaneously.
- Hospital crowding and ED boarding lead to delayed triage and inefficient ED throughput, which compromises patient safety.
- Rapid visual assessment, split flow models, and rapid medical evaluations can improve ED throughput and improve patient safety.
- Determination of the extent and severity of intestinal ischemia—and thus its treatment and prognosis—usually requires examination of the intestines during an operation.
Liliya Klimkiv, MD
Resident Physician
Department of Emergency Medicine
UC Davis Health
lvvorontsov@ucdavis.edu
Garth Utter, MD, MSc
Consulting Editor, AHRQ’s Patient Safety Network (PSNet)
Professor
Department of Surgery
Division of Trauma, Acute Care Surgery, and Surgical Critical Care
UC Davis Health
ghutter@ucdavis.edu
David K. Barnes, MD, FACEP
Consulting Editor, AHRQ’s Patient Safety Network (PSNet)
Health Sciences Clinical Professor
Department of Emergency Medicine
UC Davis Health
dbarnes@ucdavis.edu
References
- Kundan M, Chebrolu H, Muniswamppa C, et al. Outcomes of management of patients with acute mesenteric ischemia: a prospective study. Niger J Surg. 2021;27(1):16-21. [Free full text]
- Leuthauser A, McVane B. Abdominal pain in the geriatric patient. Emerg Med Clin North Am. 2016;34(2):363-375. [Available at]
- Magidson PD, Martinez JP. Abdominal Pain in the Geriatric Patient. Emerg Med Clin North Am. 2016 Aug;34(3):559-574. [Available at]
- Blomaard LC, Speksnijder C, Lucke JA, et al. Geriatric screening, triage urgency, and 30-Day mortality in older emergency department patients. J Am Geriatr Soc. 2020;68(8):1755-1762. [Free full text]
- Lyon C, Clark DC. Diagnosis of acute abdominal pain in older patients. Am Fam Physician. 2006;74(9):1537-1544. [Free full text]
- Millet I, Sebbane M, Molinari N, et al. Systematic unenhanced CT for acute abdominal symptoms in the elderly patients improves both emergency department diagnosis and prompt clinical management. Eur Radiol. 2017;27(2):868-877. [Free full text]
- Gilboy N, Tanabe P, Travers D, et al. Emergency Severity Index (ESI): a Triage Tool for Emergency Department Care, Version 4. 2020:1-114. [Free full text]
- Yancey CC, O'Rourke MC. Emergency Department Triage. In: StatPearls. Treasure Island (FL): StatPearls Publishing; August 31, 2022. [Free full text]
- Platts-Mills TF, Travers D, Biese K, et al. Accuracy of the Emergency Severity Index triage instrument for identifying elder emergency department patients receiving an immediate life-saving intervention. Acad Emerg Med. 2010;17(3):238-243. [Free full text]
- Savioli G, Ceresa IF, Gri N, et al. Emergency department overcrowding: understanding the factors to find corresponding solutions. J Pers Med. 2022;12(2):279. [Free full text]
- Jones S, Moulton C, Swift S, et al. Association between delays to patient admission from the emergency department and all-cause 30-day mortality. Emerg Med J. 2022 Mar;39(3):168-173. [Free full text]
- Badr S, Nyce A, Awan T, et al. Measures of emergency department crowding, a systematic review. How to make sense of a long list. Open Access Emerg Med. 2022 Jan 4;14:5-14. [Free full text]
- Epstein SK, Huckins DS, Liu SW, et al. Emergency department crowding and risk of preventable medical errors. Intern Emerg Med. 2012;7(2):173–80. [Free full text]
- Gorski JK, Arnold TS, Usiak H, et al. Crowding is the strongest predictor of left without being seen risk in a pediatric emergency department. Am J Emerg Med. 2021;48:73-78. [Free full text]
- Hsia RY, Sarkar N, Shen YC. Is inpatient volume or emergency department crowding a greater driver of ambulance diversion? Health Aff (Millwood). 2018;37(7):1115-1122. [Free full text]
- Yarmohammadian MH, Rezaei F, Haghshenas A, et al. Overcrowding in emergency departments: a review of strategies to decrease future challenges. J Res Med Sci. 2017;22:23. [Free full text]
- Sanchez M, Smally AJ, Grant RJ, et al. Effects of a fast-track area on emergency department performance. J Emerg Med. 2006;31(1):117-120. [Available at]
- Wallingford G Jr, Joshi N, Callagy P, et al. Introduction of a horizontal and vertical split flow model of emergency department patients as a response to overcrowding. J Emerg Nurs. 2018;44(4):345-352. [Available at]
- Gasperini B, Pierri F, Espinosa E, et al. Is the fast-track process efficient and safe for older adults admitted to the emergency department?. BMC Geriatr. 2020;20(1):154. [Free full text]
- Furmaga J, Courtney DM, Lehmann CU, et al. Improving emergency department documentation with noninterruptive clinical decision support: an open-label, randomized clinical efficacy trial. Acad Emerg Med. 2022;29(2):228-230. [Free full text]
- Corl K. “Hospitals’ new emergency department triage systems boost profits but compromise care.” STAT News: First Opinion. Published September 5, 2019. [Available at]
- Emergency Department Crowding: High Impact Solutions. American College of Emergency Physicians, Emergency Medicine Practice Committee. May 2016. Accessed August 31, 2023. [Free full text]
- Kärkkäinen JM, Acosta S. Acute mesenteric ischemia (part I) - Incidence, etiologies, and how to improve early diagnosis. Best Pract Res Clin Gastroenterol. 2017;31(1):15-25. [Available at]
- Messing B, Crenn P, Beau P, et al. Long-term survival and parenteral nutrition dependence in adult patients with the short bowel syndrome. Gastroenterology. 1999;117(5):1043-1050. [Free full text]
- Amiot A, Messing B, Corcos O, et al. Determinants of home parenteral nutrition dependence and survival of 268 patients with non-malignant short bowel syndrome. Clin Nutr. 2013;32(3):368-374. [Available at]