Failure to Latch
Rodriguez M, Mannel R, Frye DR. Failure to Latch. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2008.
Rodriguez M, Mannel R, Frye DR. Failure to Latch. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2008.
The Case
The patient is a full-term, 8.5-pound, healthy infant whose parents were strongly committed to breastfeeding exclusively for 6 months. However, early breastfeeding did not go smoothly. The newborn suckled frequently and strongly but did not appear to be receiving adequate intake. The infant had marginal output characterized by decreased urinary output, and the mother experienced painful bleeding nipples. While not specifically trained to assist with breastfeeding, nurses in the postpartum unit offered assistance but ultimately suggested formula supplementation, which the parents refused. Mother and infant were discharged 48 hours after delivery.
Because of the low output and rising bilirubin, the infant was seen by a pediatrician three times in the next 6 days and experienced a 15% weight loss. The infant's output continued to be marginal. The infant was nursing frequently for 30–45 minutes at a time, was quite fussy, and tended to fall asleep at the breast. The mother reported that her breasts were tender and the nipples were painful but no longer bleeding. The pediatrician evaluated the infant for hyperbilirubinemia (bilirubin increased to 16 mg/L) but did not observe the infant feeding. The pediatrician suggested that the parents give the infant formula supplementation before every feeding.
The worried and exhausted parents, bewildered by conflicting advice, eventually sought telephone advice from a lactation consultant, who recommended a plan of pumping, nursing, and formula supplementation after feeding. Following this regimen, the infant gained 4 ounces in 4 days and the total serum bilirubin decreased to 11. Breastfeeding continued to be difficult, and the parents scheduled a face-to-face visit with the lactation consultant. The consultant observed a feeding and performed a physical examination, after which she identified the infant as having ankyloglossia (tongue-tie).
The Commentary
This case represents a classic example of the difficulties families face when they encounter breastfeeding challenges, compounded by conflicting messages and a delayed face-to-face meeting with a health care provider. The success of breastfeeding depends on many factors; thus, it is important to ensure provision of evidence-based care to breastfeeding families. The American Academy of Pediatrics (AAP) policy statement defines "exclusive breastfeeding [as] the reference or normative model against which all alternative feeding methods must be measured with regard to growth, health, development, and all other short- and long-term outcomes."(1) Despite efforts to increase the rate of breastfeeding, only slight gains have been made.(2) During the hospital stay, 75% of infants in the United States are breastfeeding to some extent. However, this proportion falls rapidly over the first few weeks of life, and by 6 months less than 40% of infants are still breastfeeding to any degree. While the AAP and World Health Organization recommend exclusive breastfeeding for 6 months, only 11% of infants in the United States reach this target. Obstacles to achieving this goal are numerous (1,3):
- Inadequate prenatal education and postnatal support;
- Inadequate physician and staff education;
- Disruptive hospital policies and practices;
- Lack of access to international board-certified lactation consultants (IBCLCs);
- Promotion of commercial formulas;
- Lack of timely postdischarge follow-ups.
Studies have documented physicians' lack of knowledge about breastfeeding.(4) The presented case demonstrates how a physician's behavior can affect the success of breastfeeding. The presence of significant hyperbilirubinemia accompanied by a 15% weight loss at 6 days of life points to inadequate intake of breast milk and associated dehydration. Clearly, in this scenario, the appropriate action would have been an early face-to-face assessment and physical exam to identify potential issues with infant feeding and/or maternal milk supply. Such a meeting would have facilitated the development of a plan to ensure adequate infant intake while maintaining or increasing breast milk production. Best practices for overcoming breastfeeding difficulties are shown in Table 1.
Jaundice occurs in 40%–60% of newborns and is typically benign. Under certain circumstances, though, hyperbilirubinemia can become severe and place newborns at risk for hyperbilirubinemic encephalopathy and its long-term neurologic consequences. Because of this, the Joint Commission has identified kernicterus as a "never event." In 2006, the AAP published revised guidelines for managing hyperbilirubinemia in newborns by calling for risk assessment of all newborns and early follow-up after hospital discharge.(5) Infants that are breastfed will run higher bilirubin values when compared with formula-fed infants. Table 2 highlights one hospital system's strategy for managing hyperbilirubinemia.
The distinction between breast milk jaundice and "breastfeeding" jaundice is important. The former, breast milk jaundice, is an exaggerated physiologic response, occurring in approximately 2% of breastfed newborns. The etiology is not entirely clear, although the presence of glucuronidase in breast milk may play a role.(6) "Breastfeeding" jaundice is a result of caloric deprivation and increased enterohepatic circulation, sometimes called starvation jaundice, aggravated by inadequate milk intake secondary to poor breastfeeding.(7) It typically occurs during the first week of life, and infants may present with weight loss, dehydration, and inadequate stool or urine output, while the mother will have a compromised milk production.
The clinical management also differs in addressing the distinction.
- In breast milk jaundice, the infants are often thriving while presenting with sustained high bilirubin levels; the mother typically has a good milk supply. In this setting, the goal is to avoid unnecessary interruption of breastfeeding while monitoring bilirubin levels. Some clinicians will interrupt breastfeeding for 12 hours to diagnose and then resume breastfeeding while continuing to monitor. The mother should initiate milk expression with any interruption of breastfeeding. Weaning the infant completely is not recommended.
- In "breastfeeding" jaundice, the infants may present with weight loss, dehydration, inadequate stool or urine output, and the mother with associated compromised milk production. The key distinction is that these infants are not thriving. Here, the goal is to address the underlying difficulty affecting the infant's ability to latch to the mother's breast, or the reasons for the inadequate breast milk production in the mother. In addressing the infant's clinical status, the clinician should attempt to increase infant intake of any available breast milk and supplement with formula as needed. Providing support and close follow-up during this process is key to the health of the infant and successful continuation of breastfeeding.
This family's insistence that the infant's breastfeeding difficulties be addressed ultimately led to the correct diagnosis, pointing out the importance of listening to patient and family concerns. In particular, the family appeared to be skeptical of the initial determination that the problem was an underproduction of mother's milk.(8) Before determining that a mother cannot produce enough breast milk, the following factors must be excluded: (i) problems with feeding techniques such as inadequate latch-on (9); (ii) external factors such as delayed initiation or separation of mother and infant (10); and (iii) physical factors of the infant or mother that interfere with milk transfer (anatomical, neurological, etc.).(9)
Ultimately, the in-person assessment was crucial to coming to the correct diagnosis. Recommending that the mother pump and feed her breast milk allowed for the exclusion of inadequate breast milk supply, while the face-to-face visit provided for an assessment of the latching process, which was key in identifying the presence of ankyloglossia.
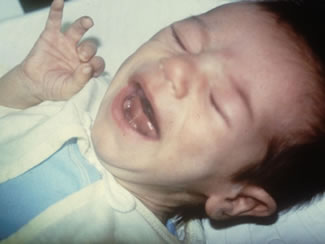
Ankyloglossia (tongue-tie) is a condition in which the bottom of the tongue is tethered to the floor of the mouth by a membrane (frenulum), thereby limiting the range of motion of the tongue (Figure). The condition is frequently familial and may result in feeding, speech, and swallowing problems. Lactation specialists recognize tongue-tie as a cause of breastfeeding difficulties.(11) The diagnosis is made by history and observation of both the infant latching and assessment of range of motion of the tongue. The reported incidence of ankyloglossia ranges from 1 in 20 to 1 in 500, and a fair amount of suspicion is required in making the diagnosis. The combination of difficulty in sucking, poor weight gain, and painful nursing should lead the pediatrician to suspect ankyloglossia during their newborn follow-up. The treatment—frenotomy—is a simple, safe, and effective surgical procedure. A snip of the tethered frenulum with blunt-ended scissors is usually all that is needed, and bleeding is minimal.(12,13)
The first 2 weeks after birth are crucial for establishing breastfeeding. Continued milk production is dependent upon regular and thorough milk removal, which does not occur when formula supplementation is the only intervention recommended. Maternal motivation, along with skilled support, are critical success factors.(3) At the same time, the health impact of breastfeeding is overwhelming.(14) Breastfeeding enhances maternal-infant bonding, diminishes risk of serious atopic disease, and protects infants from a number of illnesses. For example, infants fed formula in the first 4 months of life have a higher prevalence of diarrhea, otitis media, pneumonia, and bacteremia when compared with infants exclusively breastfed in the first 6 months of life. Infants who are not breastfed also have a higher risk of developing obesity and diabetes.
With a team effort on the part of knowledgeable health care providers, both in the hospital and in the community, issues with hyperbilirubinemia and breastfeeding difficulties can be overcome.(15) Increasing breastfeeding duration rates will significantly improve the health of our society.(14) In this case, the mother's knowledge of the benefits of breastfeeding and her persistence ultimately allowed for the correct diagnosis and management of the breastfeeding issues, ankyloglossia, and hyperbilirubinemia, despite the obstacles she confronted.
Take-Home Points
- Ensure adequate lactation education of hospital staff.
- Follow AAP guidelines in scheduling and providing for early follow-up of newborns, during which time the infant's weight and output (urine and stool) are reviewed and a thorough breastfeeding assessment completed.
- Refer mother/infant couplets with any breastfeeding difficulties to an IBCLC.
- Any intervention to increase infant intake should include a plan to protect or increase maternal milk production.
- A known cause of breastfeeding difficulties, ankyloglossia can result in painful breastfeeding, inadequate intake, jaundice, low milk production, poor weight gain, and ultimately premature weaning. Early frenotomy can prevent this series of adverse events.
Mitch Rodriguez, MD, MBA Regional Perinatal Director, Neonatal Services
Macon, Georgia Clinical Associate Professor
Department of Pediatrics
Mercer University Medical School
Rebecca Mannel, BS, IBCLC Lactation Center Manager
Oklahoma University Medical Center Hospital Corporation of America, Inc.
Donna Frye, RN, MN Clinical Director
Women's and Children's Clinical Services Hospital Corporation of America, Inc.
References
1. Gartner LM, Morton J, Lawrence RA, et al. Breastfeeding and the use of human milk. Pediatrics. 2005;115:496-506. [go to PubMed]
2. Breastfeeding. Center for Disease Control and Prevention Web site. Available at: www.cdc.gov/breastfeeding.
3. Shealy KR, Li R, Benton-Davis S, Grummer-Strawn LM. The CDC Guide to Breastfeeding Interventions. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2005. Available at: http://www.cdc.gov/breastfeeding/pdf/breastfeeding_interventions.pdf
4. Schanler RJ, O'Connor KG, Lawrence RA. Pediatricians' practices and attitudes regarding breastfeeding promotion. Pediatrics. 1999;103:E35. [go to PubMed]
5. American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2004;114:297-316. [go to PubMed]
6. Hintz SR, Gaylord TD, Oh W, et al. Serum bilirubin levels at 72 hours by selected characteristics in breastfed and formula-fed term infants delivered by cesarean section. Acta Paediatr. 2001;90:776-781. [go to PubMed]
7. Yamauchi Y, Yamanouchi I. Breast-feeding frequency during the first 24 hours after birth in full-term neonates. Pediatrics. 1990;86:171-175. [go to PubMed]
8. Nommsen-Rivers LA, Heinig MJ, Cohen RJ, Dewey KG. Newborn wet and soiled diaper counts and timing of onset of lactation as indicators of breastfeeding inadequacy. J Hum Lact. 2008;24:27-33. [go to PubMed]
9. International Lactation Consultant Association. Clinical Guidelines for the Establishment of Exclusive Breastfeeding. Raleigh, NC: U.S. Department of Health and Human Services, Maternal and Child Health Bureau; 2005. Available at: http://www.ilca.org/ClinicalGuidelines2005.pdf.
10. Evidence for the Ten Steps to Successful Breastfeeding. Geneva, Switzerland: World Health Organization, Division of Child Health and Development; 1998. ISBN: 9241591544. Available at: http://whqlibdoc.who.int/publications/2004/9241591544_eng.pdf.
11. Coryllos E, Genna CW, Salloum AC. Congenital tongue-tie and its impact on breastfeeding. American Academy of Pediatrics Newsletter. Summer 2004:1-5. Available at: http://www.aap.org/breastfeeding/8-27%20Newsletter.pdf.
12. Ballard J, Chantry C, Howard CR; for Academy of Breastfeeding Medicine Protocol Committee. Clinical Protocol #11: Guidelines for the Evaluation and Management of Neonatal Ankyloglossia and its Complications in the Breastfeeding Dyad. New Rochelle, NY: Academy of Breastfeeding Medicine; 2004. Available at: http://www.bfmed.org/ace-files/protocol/ankyloglossiaFinal_11.pdf.
13. Geddes DT, Langton DB, Gollow I, et al. Frenulotomy for breastfeeding infants with ankyloglossia: effect on milk removal and sucking mechanism as imaged by ultrasound. Pediatrics. 2008;122:e188-e194. [go to PubMed]
14. Ip S, Chung M, Raman G, et al. Breastfeeding and Maternal and Infant Health Outcomes in Developed Countries. Evidence Report/Technology Assessment No. 153. Rockville, MD: Agency for Healthcare Research and Quality; April 2007. AHRQ Publication No. 07-E007. [go to PubMed]
15. Murray EK, Ricketts S, Dellaport J. Hospital practices that increase breastfeeding duration: results from a population-based study. Birth. 2007;34:202-211. [go to PubMed]
Tables
Table 1. Best Practices Approach for Overcoming Breastfeeding Difficulties (3,9,10,12).
| • Mother and baby skin to skin during the first hour after delivery, providing the opportunity to "latch on." |
| • Early assessment by a nurse trained in basic breastfeeding management to identify latching difficulty. |
| • Referral to an IBCLC with a visit occurring within the first 24 hours. |
| • Instructions to the mother in the first 24 hours to supplement the infant with expressed milk until resolution of the breastfeeding issue. |
| • IBCLC evaluation of the latching difficulty and maternal nipple pain with identification of ankyloglossia. |
| • Development of a plan with the mother for maintaining milk production and adequate infant intake before and after hospital discharge. |
| • Access to an appropriate breast pump. |
| • Early physician referral for evaluation and possible frenotomy. |
| • Early physician follow-up to monitor hyperbilirubinemia. |
| • IBCLC follow-up after discharge to resolve nipple pain and ensure adequate infant weight gain and continued milk production. |
Table 2. A Multi-Hospital System's* Successful Approach to Support for Breastfeeding and Management of Hyperbilirubinemia to Prevent Kernicterus.
| • Objective assessment of each neonate for hyperbilirubinemia with a serum value or transcutaneous meter reading. The value is plotted on a nomogram by hour of life to determine the risk of severe hyperbilirubinemia or kernicterus. |
| • Education regarding the management of hyperbilirubinemia for health care professionals and family members. |
| • Lactation support in the form of evidence-based protocols, education for health care providers and families, and lactation support with access to board-certified lactation consultants. |
| • Equipment to assess and manage hyperbilirubinemia. |
| • Support of early newborn follow-up after discharge. |
Figure
Figure. Ankyloglossia. The bottom of the tongue is tethered to the floor of the mouth by the frenulum.