Responding to Patient Safety Events
Background
Patient safety events that occur in health care facilities require prompt action to ensure that further harm is mitigated, and future errors are prevented. Using a standardized and robust organizational approach to respond to such events promotes a culture of patient safety. Steps in responding to patient safety events include reporting, investigation, communication, remediation, data tracking, and system improvement (see Figure). This Patient Safety Primer will focus on communication, remediation, and system improvement. Event reporting, investigation, and data tracking have been described in other primers.
Figure. Key Steps in Responding to Patient Safety Events
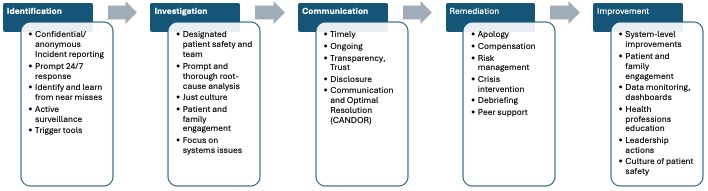
Source: McDonald TB, Helmchen LA, Smith KM, et al. Responding to patient safety incidents: the "seven pillars". Qual Saf Health Care. 2010;19(6):e11. [Free full text]
Communication and Remediation
Ongoing and timely communication with healthcare staff, patients, and families involved in the event promotes transparency and establishes trust. Such communication includes key facts, results of the root cause analysis and other investigations into the adverse event, and any improvements made to patient safety. Based on the investigation, if harm is deemed to be due to inappropriate care, the circumstances and the mechanism of harm are disclosed to the patient and family, ideally involving a trained patient liaison to help address subsequent concerns.
The Agency for Healthcare Research and Quality (AHRQ) Communication and Optimal Resolution (CANDOR) toolkit is helpful in addressing disclosure communication. It highlights that disclosure is an ongoing process that starts with an initial conversation after an event and includes full disclosure after the event investigation and analysis is completed. Patients and families report that the content of disclosure that matters most to them includes an explanation of why the error occurred, ways the error's effects will be minimized, and steps that the organization or individual will take to prevent recurrences. The importance of error disclosure is also discussed in the Disclosure of Errors primer.
If following the investigation, the adverse event is determined to be the result of substandard care, it is important that clinicians and the health care organization apologize to the patient and their caregivers without being defensive and address any questions they may have. The timing of an apology to patients and families could be guided by an assessment of the benefits of early disclosure versus the risk of premature disclosure of conclusions that may later be erroneous. As described in the CANDOR toolkit, components of an apology should include acknowledging the gaps in care, taking responsibility for them, and empathetically and genuinely expressing remorse. If indicated, early compensation could occur in the form of waiving hospital bills while the healthcare organization works with the patient toward resolution of any financial claims.
A just culture promotes shared accountability and emphasizes that safety events are usually a product of system failures at healthcare organizations, rather than solely individual staff behaviors. Timely communication of key facts with healthcare staff should be done with objectivity and compassion guided by principles of just culture, acknowledging that patient safety events stem from interactions between humans and the complex systems in which they perform their tasks. In the aftermath of a patient safety event, healthcare staff involved could face feelings of guilt, inadequacy, or anguish. Staff involved may feel personally responsible for the patient safety event and question their own knowledge and skills. This especially tends to occur in situations where the healthcare staff bonds with a patient or family or in cases where there is sudden unexpected demise of a patient. For more information, see related primer, Second Victims: Support for Clinicians Involved in Errors and Adverse Events.
The CANDOR framework describes three tiers of support when developing a peer support program in healthcare organizations: department or unit support from supervisors and fellow team members, trained peer supporters and risk management resources to provide crisis intervention, and debriefing and expedited professional support and guidance from employee assistance programs, psychologists, or social workers. Addressing professional suffering by developing an infrastructure for robust and rapid individual and team support facilitates the coping and recovery process for members of the healthcare team.
System Improvement
Critical aspects of responding to patient safety events is a focus on systems issues that need to be changed, acknowledging the impact on healthcare staff, and identifying individuals who need further support. Establishing consistent behavioral standards for all employees and establishing clarity around roles, expectations, and accountability promotes a just culture. If no harm to patients resulted, the incident is typically classified as a near miss or close call and should undergo further evaluation. Near misses are significantly more common than adverse events and can shine a light on potential safety hazards. They provide an opportunity for organizational learning if accompanied by system-level actions and change.
A necessary next step is identifying and implementing system-level improvements to address latent errors and prevent recurrence of similar system failures in the future. Latent errors are less obvious system failures that contribute to patient safety events and are referred to as “accidents waiting to happen”. Involving patients and families in improvement efforts enables user-centered design of potential solutions. Selecting relevant quality measures and ongoing collection, tracking, and evaluation of data to assess the effectiveness of improvement efforts is essential for quality assurance and public outreach. The structured use of data and dashboards to monitor, compare, benchmark, and evaluate patient safety trends helps sustain improvements and implement ongoing steps to minimize the likelihood of a similar patient safety event occurring in the future.
Other improvement efforts include continuing education of health professionals through simulation, morbidity and mortality rounds, and disclosure training. Closing the safety action feedback loop where the reporter of a patient safety event and other relevant healthcare staff are informed of interventions and improvements promotes organizational learning. Finally, health system leadership that prioritizes patient safety by setting data-informed safety goals, promptly responding to healthcare staff and patient concerns, supporting and role-modeling efforts to improve safety, and continually monitoring and disseminating progress promotes an ongoing culture of safety.
The approach of responding to patient safety events to prevent future errors is referred to as Safety-I. Combining this response to patient safety events with a proactive approach, Safety-II, where aspects of care that went well are identified and used to standardize and scale up best practices, can promote sustainable improvements in patient safety and resilient healthcare. This complementary approach incorporates the understanding that healthcare is a complex adaptive system where clinicians may need to adopt standardized processes with appropriate adjustments in their workflow to meet the dynamic and evolving needs of people seeking care.
Ulfat Shaikh, MD, MPH, MS
Associate Editor, AHRQ's Patient Safety Network (PSNet)
Professor of Pediatrics and Medical Director for Healthcare Quality
UC Davis Health
ushaikh@ucdavis.edu



