CVC Placement: Speak Now or Do Not Use the Line
Ault M, Rosen B. CVC Placement: Speak Now or Do Not Use the Line. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2013.
Ault M, Rosen B. CVC Placement: Speak Now or Do Not Use the Line. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2013.
The Case
A 48-year-old woman with a history of hypertension, psychiatric illness, and a previous suicide attempt overdosed on her blood pressure medication (calcium channel blocker). When found unresponsive by her partner on the bathroom floor, she was brought by ambulance to the emergency department (ED). A right subclavian central line was placed during resuscitation.
No blood return was obtained from any of the lines. The ED team thought this was likely due to severe hypotension (her systolic blood pressure was around 50 mm Hg), but there was some concern that the line was not in the proper position. A chest radiograph was obtained when the patient arrived in the intensive care unit (ICU). The initial reading noted that the line might have been in the right atrium (which is to say, inserted too far). However, the radiology attending physician concluded the line was in good position.
Reassured, the line was used by the cardiology team to deliver medications and fluids during pacemaker insertion. Several hours later, a repeat chest radiograph was ordered after the patient began to vomit. This radiograph showed whiteout of the right lung, and ultimately the clinicians realized that the tip of the subclavian line was actually within the lung. Approximately 1400 cc of fluid was then removed from her pleural space via thoracentesis. Fortunately, the patient made a full recovery.
The Commentary
Central venous catheter (CVC) placement is one of the most common medical procedures performed in health care today. Nearly 5 million CVCs are routinely placed each year for infusion, phlebotomy, and/or hemodynamic monitoring.(1) Although overall complication rates for CVC insertion should be exceedingly low, published complication rates vary considerably and have been reported as high as 19% (Table). The possibilities for harm are numerous and include accidental trauma to non-venous structures (arteries, lung, nerve, visceral organs); bleeding (hematoma, hemothorax, or hemorrhage); operator injury (needle stick or splash); and catheter-related issues (retained wire, bloodstream infections, sheared catheter, dysrhythmias, thrombosis, through-and-through vessel trauma, or, as in this case, malpositioning). There is controversy over which vein is "best." The subclavian vein is recommended by the Institute for Healthcare Improvement due to the presumed lower infection rates associated with this positioning; however, procedural complications may be more common with this vein because of its anatomic proximity to the chest cavity and lungs.(2,3) The exact opposite may be true for femoral veins.
Highlighted in this case is an example of a three-faceted CVC error resulting in significant iatrogenic harm to an already critically ill patient. Identified concerns include: (i) improper insertion technique (real-time ultrasound not utilized); (ii) improper decision to use the line, despite inability to withdraw blood from it; and (iii) poor handoff communication between the different treatment teams.
Error #1
Best practice for CVC placement mandates the use of ultrasound as a critical element for safety.(4,5) In fact, the Agency for Healthcare Research and Quality (AHRQ) has been recommending the use of ultrasound guidance (UG) for more than 10 years.(6) In addition, the 2011 Centers for Disease Control and Prevention (CDC) guidelines recommend using UG to place CVCs to reduce the number of cannulation attempts and mechanical complications (Category 1B). The medical community appears to be adopting these guidelines, albeit slowly. A 2005 survey of medicine housestaff at Vanderbilt demonstrated that only 15% were using UG on at least 60% of CVC attempts.(7) A more recent study of 113 emergency department (ED) physicians showed that 97% of respondents have access to an ultrasound machine in their ED, but that only 78% (n = 88) of respondents indicated that they perform UG CVC placement. Furthermore, 26% (n = 28) of those respondents stated they felt "uncomfortable" or "very uncomfortable" with UG CVC placement. Even among those who had been trained in UG CVC placement, 13% (95% confidence interval [CI]: 7%–22%) still reported being "uncomfortable" or "very uncomfortable" with the technique (P 8) Our own informal experiences surveying participants at the annual Society of Hospital Medicine Procedure Pre-Courses (which we have been coordinating since 2008) tell us that familiarity with ultrasound has improved over the years. However, as recently as April 2012 no more than 50% of participants either have easy access to, or are regularly using, UG for CVC placement.
Most commonly cited barriers to more widespread ultrasound use include lack of easy access to an ultrasound machine, a shortage of structured training and educational opportunities for clinicians, perceived lack of time for use in emergent situations, and cultural resistance to change.
The fundamental requisite to ensuring the safe placement of a CVC is proper operator experience and/or supervision. The time honored "see one, do one, teach one" method is inadequate in today's environment—in fact, the mantra "practice, practice, practice" is more applicable. Evidence suggests that operators who have placed at least 50 central lines have fewer complications than those with less experience.(9) To that end, the use of simulators has greatly expanded and is now becoming the preferred training approach. Use of simulators allows for a no-risk, low-stress environment for trainees to learn the equipment and practice the procedure, develop muscle memory for the key technical steps, and demonstrate proper safety practices (hand hygiene, wide sterile barriers, and sharps safety). Nonhuman tissue-based simulator training has been shown to increase trainees' level of comfort and perceived readiness for attempts on real patients, as well as significantly improve objective performance abilities for key elements of central line placement.(10,11) Additionally, the practice of simulation-based mastery training for already credentialed practitioners not only reduces mechanical complications of insertion but also significantly decreases central line–related infections.(12)
Training with a proceduralist on a Procedure Service is another excellent adjunctive training option because it enables the trainee to learn procedures incrementally, with hands-on support during the more challenging stages of the procedure, and progressive hands-off supervision as skills are mastered. Development of these services in academic/teaching institutions is growing and has been effective in providing resident training.(13,14) In terms of direct patient care by dedicated proceduralists, our own data (manuscript pending) has shown that a small cadre of high-volume proceduralists consistently cause fewer complications than rates in the published literature for the most common medical procedure.(15) We are anecdotally aware of several institutions that have (or will soon have) established similar procedure services for direct patient care and/or for training purposes, although how widespread this approach will be remains to be seen.
Error #2
Confirmation of proper CVC positioning prior to using the device is of equal importance. The optimal position for the catheter tip placed in the subclavian or internal jugular vein is at the junction of the superior vena cava (SVC) and right atrium (the cavoatrial junction). For this purpose, chest radiographs play an essential role. However, the operator should use these static pictures only as supplementary information. The most fundamental technique for placement confirmation is for the operator to be able to aspirate blood from, and flush saline into, all of the CVC's lumens. Inability to withdraw blood from any of the ports of a line is an ominous sign, as it indicates a potential blockage or disconnect between the catheter port and intraluminal space. Despite the clinicians' rationale in this case, the ability to aspirate or flush is not affected by volume status or hemodynamic stability (unless the patient has completely exsanguinated), and thus should not have been reassuring.
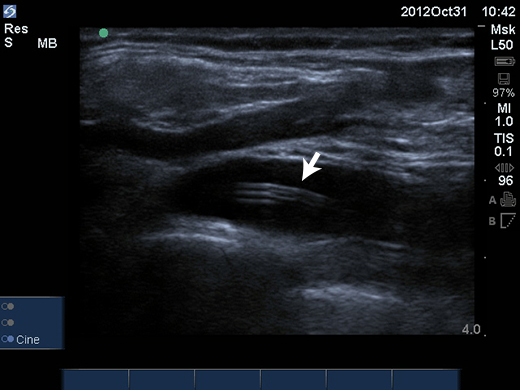
Along with its crucial role in proper line placement, ultrasound can also help ensure correct intraluminal (venous) placement and evaluate the errant placement of a catheter. The same high-frequency linear (vascular) probe recommended for CVC placement can also be used to obtain an image of the catheter within the vein (Figures 1,2). Advanced protocols have been developed to immediately confirm tip location in the SVC by interrogating the internal jugular and subclavian veins and obtaining cardiac views of the cavoatrial junction with the low-frequency phased array probe—these techniques can be 93%–96% accurate, reduce confirmation time from 70–80 minutes (for chest radiograph) to 10 minutes using ultrasound, and allow for immediate identification of pneumothorax.(16,17)
Error #3
Robust communication and handoffs between services is key to patient safety and, in the case of a newly placed CVC, can mean the difference between life and death. Answer questions such as: Was the catheter placed under sterile or emergent conditions? Was ultrasound used? Was blood aspiration and flushing achieved? Has placement been confirmed? How many attempts were made before achieving access? Experience with the Pronovost checklist has taught us that "it takes a village" to provide optimal line care safety.(18) In this case, there was likely a communication breakdown between the ED, radiology, the ICU team, and the cardiologists. Proper communication during handoffs may have led to further investigation of the line integrity prior to usage.
Conclusion
The placement of CVCs is fundamentally safe, vitally important, and commonly performed in the hospitalized patient. However, a number of potential complications can occur over the entire life of the catheter if proper protocols are not followed. Insistence on adequate training, strict adherence to fundamental insertion principles, and robust communication between services help ensure first-rate patient care. If clinicians have any doubt along the way, it is incumbent on them to "speak now or do not use the line" (as the title of this case suggests).
Take-Home Points
- Use of ultrasound for placement and evaluation of line position is an essential, critical safety element for safe CVC placement.
- Successful aspiration of blood from a new CVC is an essential (but not sufficient) confirmation step prior to using the line.
- As with any aspect of modern medicine, we must guard against "voltage drop" of vital clinical information when patients are handed off from one team to another.
- Operator training and experience are key determinants of operator-related complications. Adequate supervision and the use of simulators are critical adjuncts to proper procedural training.
Mark Ault, MD Director, Division of General Internal Medicine Assistant Chairman for Clinical Affairs, Department of Medicine Cedars-Sinai Medical Center
Bradley Rosen, MD, MBA Medical Director, Inpatient Specialty Program Cedars-Sinai Medical Center
References
1. Kondro W. Alberta retreats over sterilisation compensation. Lancet. 1998;351:892. [go to PubMed]
2. McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med. 2003;348:1123-1133. [go to PubMed]
3. Eisen LA, Narasimhan M, Berger JS, Mayo PH, Rosen MJ, Schneider RF. Mechanical complications of central venous catheters. J Intensive Care Med. 2006;21:40-46. [go to PubMed]
4. Randolph AG, Cook DJ, Gonzales CA, Pribble CG. Ultrasound guidance for placement of central venous catheters: a meta-analysis of the literature. Crit Care Med. 1996;24:2053-2058. [go to PubMed]
5. Fragou M, Gravvanis A, Dimitriou V, et al. Real-time ultrasound-guided subclavian vein cannulation versus the landmark method in critical care patients: a prospective randomized study. Crit Care Med. 2011;39:1607-1612. [go to PubMed]
6. Making Health Care Safer: a Critical Analysis of Patient Safety Practices: Summary. Evidence Report/Technology Assessment No. 43. [Available at]
7. Girard TD, Schectman JM. Ultrasound guidance during central venous catheterization: a survey of use by house staff physicians. J Crit Care. 2005;20:224-229. [go to PubMed]
8. Backlund BH, Hopkins E, Kendall JL. Ultrasound guidance for central venous access by emergency physicians in Colorado. West J Emerg Med. 2012;13:320-325. [go to PubMed]
9. Sznajder JI, Zveibil FR, Bitterman H, Weiner P, Bursztein S. Central vein catheterization. Failure and complication rates by three percutaneous approaches. Arch Intern Med. 1986;146:259-261. [go to PubMed]
10. Ault MJ, Rosen BT, Ault B. The use of tissue models for vascular access training. Phase I of the Procedural Patient Safety Initiative. J Gen Intern Med. 2006;21:514-517. [go to PubMed]
11. Rosen BT, Uddin PQ, Harrington AR, Ault BW, Ault MJ. Does personalized vascular access training on a nonhuman tissue model allow for learning and retention of central line placement skills? Phase II of the Procedural Patient Safety Initiative (PPSI-II). J Hosp Med. 2009;4:423-429. [go to PubMed]
12. Barsuk JH, Cohen ER, Feinglass J, McGaghie WC, Wayne DB. Use of simulation-based education to reduce catheter-related bloodstream infections. Arch Intern Med. 2009;169:1420-1423. [go to PubMed]
13. Smith CC, Gordon CE, Feller-Kopman D, et al. Creation of an innovative inpatient medical procedure service and a method to evaluate house staff competency. J Gen Intern Med. 2004;19:510-513. [go to PubMed]
14. Lenhard A, Moallem M, Marrie RA, Becker J, Garland A. An intervention to improve procedure education for internal medicine residents. J Gen Intern Med. 2008;23:288-293. [go to PubMed]
15. Ault MJ, Rosen BT. Proceduralists—leading patient safety initiatives. N Engl J Med. 2007;356:1789-1790. [go to PubMed]
16. Vezzani A, Brusasco C, Palermo S, Launo C, Mergoni M, Corradi F. Ultrasound localization of central vein catheter and detection of postprocedural pneumothorax: an alternative to chest radiography. Crit Care Med. 2010;38:533-538. [go to PubMed]
17. Matsushima K, Frankel HL. Bedside ultrasound can safely eliminate the need for chest radiographs after central venous catheter placement: CVC sono in the surgical ICU (SICU). J Surg Res. 2010;163:155-161. [go to PubMed]
18. Pronovost P, Needham D, Berenholtz S, et al. An intervention to decrease catheter-related bloodstream infection in the ICU. N Engl J Med. 2006;355:2725-2732. [go to PubMed]
Table
Table. Frequency of Mechanical Complications, According to the Route of Catheterization.
| Complication | Frequency | ||
|---|---|---|---|
| Internal Jugular (%) | Subclavian (%) | Femoral (%) | |
| Arterial puncture | 6.3 to 9.4 | 3.1 to 4.9 | 9.0 to 15.0 |
| Hematoma | 1.2 to 2.1 | 3.8 to 4.4 | |
| Hemothorax | NA | 0.4 to 0.6 | NA |
| Pneumothorax | 1.5 to 3.1 | NA | |
| Total | 6.3 to 11.8 | 6.2 to 10.7 | 12.8 to 19.4 |
Adapted from (2) with permission from the Massachusetts Medical Society. NA = Not applicable
Figures
Figure 1. Longitudinal ultrasound view of subclavian vein, catheter (arrow), with subclavian artery above it.
Figure 2. Transverse ultrasound view of subclavian vein, with cross-section of catheter (arrow).