Glucose Roller Coaster
The Case
A 71-year-old woman with congestive heart failure was admitted to the hospital. Her medical history was significant for dialysis-dependent, end-stage kidney disease and coronary artery disease. She did not have a preadmission diagnosis of diabetes.
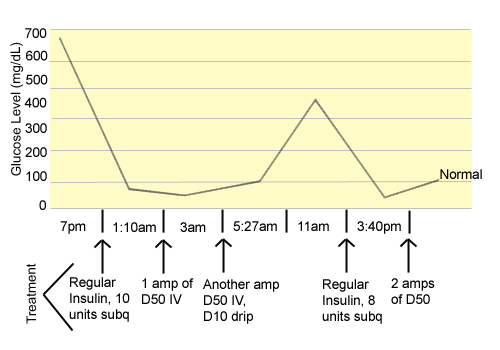
While in the step-down unit on the evening of admission, the patient had a routine phlebotomy sample drawn, and the blood sugar level was 674 mg/dL. At 11:30 pm, the nurse notified the covering intern, who telephone-ordered 10 Units of regular insulin to be given subcutaneously. At 1:10 am, a finger-stick glucose level was 50 mg/dL, and the intern verbally ordered 1 amp of D50 to be given intravenously (IV). At 3:00 am, a phlebotomized specimen revealed a glucose level of 19 mg/dL, and the intern verbally ordered another amp of D50 IV, as well as a D10 drip. At 5:27 am, a finger-stick glucose was 99 mg/dL. At 11:00 am, a phlebotomy sample revealed a blood glucose level of 351 mg/dL. Another covering intern was notified, and 8 units of regular insulin were ordered to be given subcutaneously. At 3:40 pm, the patient was unresponsive, and a finger-stick glucose level was 13 mg/dL. Two amps of D50 were verbally ordered, and follow up finger sticks were in the normal range.
Later, it was discovered that many of the phlebotomy specimens had been drawn above an IV line infusing dextrose solution. The step-down nurse was re-educated regarding blood draws in relation to lines. Despite multiple episodes of hypoglycemia, all subsequent glucose levels were normal and this patient suffered no lasting harm.
The Commentary
Although multiple factors contributed to this patient's roller coaster glycemia (Figure 1), her case highlights the challenges and perils of "cross-coverage," the management of patients by physicians other than those primarily responsible, and the limitations of "signout," the transfer of patient data and care responsibility when the primary physician goes off-duty.
From a resident's perspective, cross-coverage is hard. The most challenging aspect is obvious and inherent: residents must make clinical decisions about unfamiliar patients, often with inadequate information. Without a complete history, a physical exam, and a full assessment of a patient's problems, providing high-quality care is challenging. Published literature supports this notion: discontinuity, and by definition, cross-coverage, in the care of hospitalized patients can lead to increased lengths of stay, in-hospital complications, and preventable adverse events.(1-3)
Cross-coverage is not only inherently difficult, but it occurs when many other duties and tasks are vying for residents' attention. Cross-coverage responsibility is often added to the need to care for their patients. Alternatively, cross-coverage is sometimes organized as a stand-alone role (such as in "nightfloat"), but in these circumstances the demands are often high. On the internal medicine service at our institution, for example, the on-call interns provide some early evening coverage during the busiest admitting time of the day. Moreover, our nightfloat intern may be responsible for as many as 40-60 patients (including some in the ICU) and can expect to receive 5-20 pages per hour. Clearly, it is impossible to directly evaluate each patient or review each chart when called. Therefore, inexperienced residents are often asked to prioritize and triage patients with limited or inadequate information. We are not told in this case if the interns were sleeping in their call rooms or busy admitting patients, but it is a safe bet that they had other patient care responsibilities. In this setting, significant or potentially life-threatening problems, like hypoglycemia, are often managed over the phone, which can lead to poor outcomes, as seen here.
Cross-coverage is common in modern medical training programs. At our institution, residents spend 2-4 weeks out of each year in a cross-cover or "float" capacity; we know of other programs in which residents spend even more time in these roles. Adding up all the "floating" (particularly since the implementation of the ACGME duty hours limitations [4]), this type of duty can consume as much as 20% of a resident's inpatient training.
However, despite potential implications for patient safety and medical errors, cross-coverage is not viewed as a fundamental or core component of medical education. Residency is filled with didactics on atrial fibrillation and preeclampsia, but no structured training in efficient triage and quality care of unfamiliar patients. Nightfloat interns typically don't receive any structured orientation, and are often told to "Just keep 'em alive until the morning." When called about patients they are covering, residents and interns may view it as a nuisance or interruption in their other duties, regardless of the clinical situation. In this culture, it is not surprising that a busy intern with limited or inadequate knowledge of a 71-year-old with heart failure would be tempted to manage her care with reflexive verbal orders without a more thorough evaluation.
Minimizing patient risk in this setting is challenging. The attending could invest time teaching the interns involved about inpatient problem triage and proper signout, but reprimanding individual housestaff cannot be the only solution. Raising individual awareness about the inherent risks involved in information and patient care transfer is beneficial, but reliance on individual provider vigilance and performance has been ineffective.(5) Instead, efforts should focus on modifying the culture of cross-coverage at academic institutions. Clearly, more time and energy could be dedicated to structured training in the management of acute conditions in unfamiliar patients, as well as to patient signout.
The signout process itself can be improved. The transfer of information between two individuals, whether between control tower and pilot or two physicians, creates an opportunity for miscommunication and errors in judgment, even under the best circumstances. Adding to the risk, resident signout is often performed in a haphazard, unstructured fashion—30 seconds in an elevator or two sentences on the phone while walking out the door—which can lead to forgetfulness and error.(6) Standardization of communication, employed in the airline industry, is one potential solution. Checklists (7) and signout cards (8) may decrease the risk of error and improve the satisfaction of the housestaff. Information technology—including computerized signouts (9), an easily accessible medical record, and computerized physician order entry—can improve the quality of data transferred and allow for better informed cross-coverage.
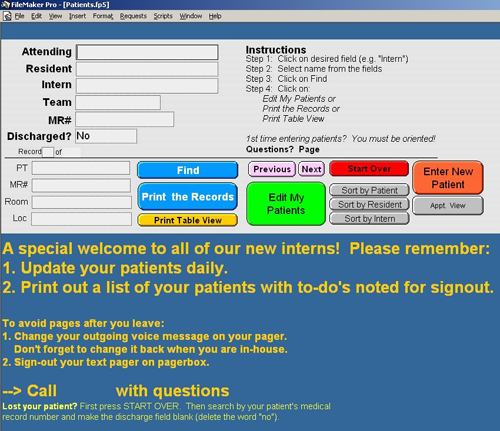
However, improving signout at an institution does not require the installation of sophisticated, complex, and expensive electronic medical records or technology. At UCSF Medical Center, for example, our full-fledged, hospital-wide computerized physician order entry system is presently being implemented. Nevertheless, we have accomplished two interventions at a reasonable cost that have markedly improved signouts and allowed housestaff to learn key information about cross-coverage patients without the ritual of rifling through stacks of index cards (assuming the cards can be located at 3 am). The first is alphanumeric text paging. Nurses and others now can easily look up residents' names on a web site, write a short message, and send it to their pagers. We estimate that 75% of pages are informational only; freeing the resident from having to stop what he or she is doing, find a phone, and return a page (which might be for anything from a "just wanted you to know that I have drawn Mr. Smith's potassium" to "Mrs. Jones looks like she might code in the next few minutes") allows the residents to prioritize their time, minimize their distractions, and provide better cross-coverage.
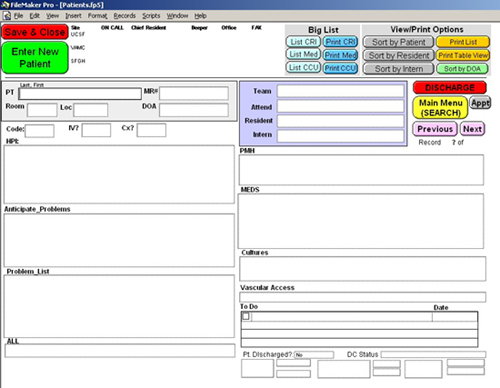
The second important intervention at our institution has been the development of a computerized signout program. Although some commercial programs are available, our residents wrote their own program in a database format. Housestaff now create and update signout sheets on every patient, and the system is available at computers around the institution. Residents can also transmit requests to schedule tests or discharge appointments to ward clerks. Figures 2 and 3 show screen shots from the system. We are in the process of migrating the system to the web, creating a portal for nurses to access the records and input requests and concerns, and allowing the system to communicate with wireless devices. Although the ideal system will link to a robust electronic medical record (and draw information like medication lists and lab results from it), this standalone system is a practical, relatively inexpensive solution to the clear and present danger of cross-coverage fumbles.
Fortunately, this patient did not suffer any long-term consequences. In this case, patient unfamiliarity, inadequate signout, time limitations, and the institutional culture surrounding cross-coverage likely influenced the interns' management. No solution is foolproof. Nonetheless, improving training in cross-coverage, standardizing the signout process, and using information technology may allow practitioners to bridge these gaps.
Take-Home Points
- New ACGME duty-hour requirements are increasing resident cross-coverage, signout, and discontinuity of care for hospitalized patients.
- Errors during cross-coverage are often due to patient unfamiliarity, other work burden, resident fatigue, and decreased supervision.
- Improving training in cross-coverage, standardizing the signout process, and using information technology may decrease the error rates of signouts.
- Although robust, institution-wide informatics solutions are ideal, alphanumeric paging and standalone signout database systems are two examples of relatively simple, inexpensive interventions that can improve signouts and cross-coverage while more expensive and complex systems are being implemented.
Bradley A. Sharpe, MD Assistant Clinical Professor Assistant Chief of the Medical Service University of California, San Francisco
References
1. Laine C, Goldman L, Soukup JR, Hayes JG. The impact of regulation restricting medical house staff working hours on the quality of patient care. JAMA. 1993;269:374-8.[ go to PubMed ]
2. Gottlieb DJ, Parenti CM, Peterson CA, Lofgren RP. Effect of a change in house staff work schedule on resource utilization and patient care. Arch Intern Med. 1991;151:2065-70.[ go to PubMed ]
3. Petersen LA, Brennan TA, O'Neil AC, Cook EF, Lee TH. Does housestaff discontinuity of care increase the risk for preventable adverse events? Ann Intern Med. 1994;121:866-72.[ go to PubMed ]
4. Vidyarthi A. Fumbled Handoff. AHRQ WebM&M [serial online]. March 2004. Available at: [ go to commentary ]. Accessed July 12, 2004.
5. Wachter RM, Shojania KG. Internal bleeding: the truth behind America's terrifying epidemic of medical mistakes. New York, NY: Rugged Land Press; 2004.
6. Coiera E, Tombs V. Communication behaviours in a hospital setting: an observational study. BMJ. 1998;316:673-6.[ go to PubMed ]
7. Jelley MJ. Tools of continuity: the content of inpatient check-out lists [Abstract]. J Gen Intern Med. 1994;9(suppl 2):77.
8. Lee LH, Levine JA, Schultz HJ. Utility of a standardized sign-out card for new medical interns. J Gen Intern Med. 1996;11:753-5.[ go to PubMed ]
9. Petersen LA, Orav EJ, Teich JM, O'Neil AC, Brennan TA. Using a computerized sign-out program to improve continuity of inpatient care and prevent adverse events. Jt Comm J Qual Improv. 1998;24:77-87.[ go to PubMed ]
Figures
Figure 1. The Glucose Roller Coaster
Figure 2. Front Page of Computerized Signout Program
Figure 3. Blank Computerized Signout Sheet